J Cardiovasc Thorac Res. 15(2):116-120.
doi: 10.34172/jcvtr.2023.31624
Short Communication
Association of the high-sensitive cardiac troponin T levels and long-term mortality in patients with acute aortic dissection type A
Yaser Jenab Conceptualization, Methodology, Supervision, Writing – original draft, Writing – review & editing, 1 
Seyed-Hossein Ahmadi-Tafti Funding acquisition, Investigation, Methodology, Visualization, 2 
Tahereh Davarpasand Data curation, Investigation, Resources, 1 
Arash Jalali Formal analysis, Validation, 1 
Hamid Khederlou Conceptualization, Project administration, Resources, Supervision, Visualization, 1, * 
Author information:
1Tehran Heart Center, Tehran University of Medical Sciences, Tehran, Iran
2Department of Cardiac Surgery, Tehran University of Medical Sciences, Tehran, Iran
Abstract
Introduction:
Acute aortic dissection type A is a life-threatening cardiovascular emergency necessitating rapid diagnosis and treatment. We sought a new prognostic tool with cardiac biomarkers and simple inflammatory factors.
Methods:
from 2003 to 2014, 50 patients with documented acute aortic dissection type A were entered to this study. These patients were followed up until December 2020; within median follow up of 93.6 months. The patients were evaluated on the association of the baseline characteristics, first laboratory investigation, echocardiographic findings, surgical approach, and long-term mortality.
Results:
Total number of mortality during the follow up was 29 (58%) patients, which was significantly higher in medical group (89.4% vs 38.7%, P value=0.001). Multivariable analysis showed only an increase in hs-cTnT levels was suggested as a predictor of mortality (95% CI: 1.06–1.38; HR=1.21; P=0.005), so that for every 100 units increase, patients were 21% more likely to have mortality in long term. Also, performing surgical treatment for aortic dissection was determined as the independent predictor of surviving, so that death was 74.6% less than those who received medical treatment (95% CI: 0.13–0.58; HR=0.27; P=0.001).
Conclusion:
hs-cTnT is a potential predictor of mortality in patients with acute aortic dissection type A.
Keywords: Cardiac Troponin, Aorta, Aortic Dissection, Mortality
Copyright and License Information
© 2023 The Author(s)
This is an open access article distributed under the terms of the Creative Commons Attribution License (
http://creativecommons.org/licenses/by/4.0/), which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited.
Introduction
There are two types of aortic dissection; type A and type B. type A, if the aortic dissection occurs in the ascending aorta and type B, if aortic dissection originates in the descending aorta.
1
Acute aortic dissection (AAD) type A is a life-threatening cardiovascular emergency, with a mortality rate of 1%–2% per hour. In spite of the advances in the diagnosis of AAD through new diagnostic imaging modalities, AAD may prove fatal if not diagnosed timely and managed appropriately.
2
Some laboratory tests such as red blood cell count, white blood cell count, cardiac troponin (cTn), and creatine kinase (CK) were recommended in the 2014 guidelines of the European Society of Cardiology (ESC) on the diagnosis and treatment of aortic disease.
3
Materials and Methods
In a cross-sectional from September 2003 to September 2014, 82 patients were admitted at Tehran heart center with AAD. 50 patients who hadn’t exclusion criteria and they have inclusion criteria entered in this study. During hospitalization, 31 (62.0%) patients underwent surgery and the remaining patients (38%) were managed conservatively with close monitoring in the intensive care unit (ICU) to control blood pressure and heart rate with Sodium Nitroprusside and Esmolol because of being high risk for surgery according to responsible surgeon decision. Two groups (medical and surgical) evaluated in term of baseline characteristics, first laboratory investigation (white blood cell, platelet counts, serum creatinine, D-dimer, and hs-cTnT), echocardiographic findings. These patients were followed up until December 2020; within median follow up of 93.6 months (Figure 1).
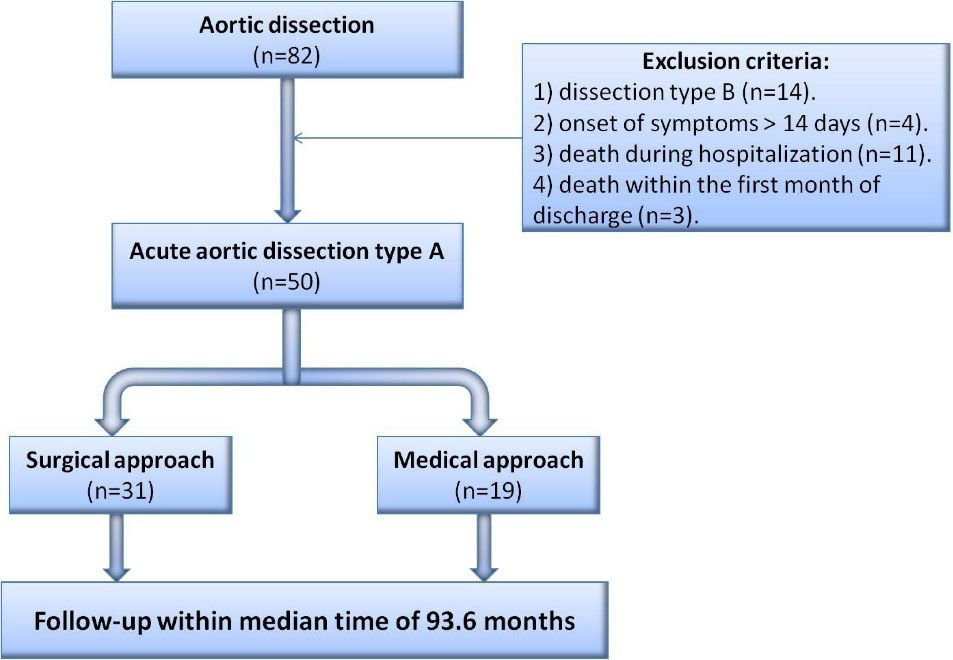
Figure 1.
Sampling flowchart of the study for evaluation of the association between High-sensitive cardiac troponin T and long-term mortality in patients with acute aortic dissection type A
.
Sampling flowchart of the study for evaluation of the association between High-sensitive cardiac troponin T and long-term mortality in patients with acute aortic dissection type A
Statistical analysis
The continuous variables are presented through means and standard deviations (SDs) or medians with interquartile ranges and were compared between the survivors and nonsurvivors using the Student t-test or the Mann–Whitney U test. The categorical variables are described as frequencies and percentages and were compared between the 2 mentioned groups using the χ2 test or the Fisher exact test. A backward logistic regression model was applied to find the multiple predictors of mortality. Variables with a P < 0.2 in the univariate analyses were candidate to enter the final model. The effect of the covariates on survival was reported as ORs with 95% CIs.
Results
Patients who received medical treatment were significantly older than patients who underwent surgery. Also, patients with a history of CAD and CVA were more likely to receive medical treatment. Patients with at least moderate AI underwent more surgery (Table 1).
Table 1.
Comparison of patients with surgical and medical treatment in terms of baseline characteristics, first laboratory investigation and echocardiographic findings
|
Variable
|
Surgical group (n=31)
|
Medical group (n=19)
|
P
-value
|
| Gender (Male) |
20 (64.50%) |
9 (47.30%) |
0.233 |
| Age |
53.06 ± 14.96 |
63.95 ± 16.15 |
0.019 |
| Limb paralysis |
3 (9.70%) |
1 (5.30%) |
0.998 |
| syncope |
4 (12.9%) |
5 (26.30%) |
0.273 |
| SBP (mmHg) |
138.90 ± 29.77 |
137.89 ± 24.21 |
0.901 |
| Heart rate (Bits/min) |
81.52 ± 17.70 |
89.05 ± 25.04 |
0.260 |
| History of aortic disease |
4 (12.90%) |
5 (26.30%) |
0273 |
| History of CAD* |
3 (9.70%) |
8 (42.10%) |
0.013 |
| History of HTN* |
18 (58.1%) |
13 (68.40%) |
0.464 |
| History of CVA* |
0 (0%) |
3 (15.80%) |
0.049 |
| History of CKD* |
1 (3.20%) |
0 (0%) |
0.998 |
| hs Troponin T level (ng/dl) |
21.49 (8.69-99.60) |
20.52 (12.69-101.60) |
0.984 |
| D-dimer level (ng/dl) |
1.70 (0.60-5.11) |
4.86 (1.70-11.80) |
0264 |
| White blood cell count ( × 10³) |
10.1 (8.70-13.01) |
12.5 (9.70-16.02) |
0.074 |
| Hemoglobin (mg/dl) |
13.03 ± 2.45 |
12.72 ± 1.93 |
0.644 |
| Platelet count ( × 10³) |
176.5 (133.20-225.40) |
162 (115.20-237.10) |
0.984 |
| Neutrophil/Lymphocyte ratio |
4.52 (2.54-8.48) |
6.01 (4.18-9.44) |
0.154 |
| Creatinine (mg/dl) |
1 (0.87-1.50) |
1.03 (0.80-1.60) |
0.952 |
| Ejection fraction (%) |
52.48 ± 9.61 |
54.37 ± 11.30 |
0.532 |
| Moderate AI ≤ |
25 (83.30%) |
11 (57.9%) |
0.049 |
| Pericardial effusion |
13 (43.30%) |
7 (36.8%) |
0.652 |
| Ascending aorta diameter (mm) |
57.80 ± 12.97 |
51.35 ± 16.48 |
0.145 |
*SBP, Systolic blood pressure; CAD, Coronary artery disease; HTN, Hypertension; CVA, Cerebrovascular arrest; CKD, Chronic kidney disease; AI, Aortic insufficiency.
Total number of mortality during the follow up was 29 (58%) patients, which was significantly higher in medical group (89.4% vs 38.7%, P-Value = 0.001) (Figure 2). Baseline characteristics of two groups (survivor and non-survivor) are depicted in Table 2. The mean age of patients was 57.2 ± 16.1 (27–84) years and more patients (58.0%) were male. The most frequent risk factor in patients with AAD type A was hypertension. A history of aortic disease or previous aortic root manipulation was positive in 9 (18.0%) patients: 1 (2.0%) patient with the Marfan syndrome, 1 (2.0%) patient with the Ehler-Danlos syndrome, 1 (2.0%) patient with aortic coarctation, 3 (6.0%) patients with a history of aortic root dilation, and 3 (6.0%) patients with a history of aortic valve replacement. There was no significant association between history of aortic disease and mortality. The mean left ventricular ejection fraction (LVEF) of the study population was 53.20% ± 10.30%. Moderate or severe aortic insufficiency (AI) and pericardial effusion were seen in 36 (73.5%) and 20 (40.8%) patients, respectively. In this study, elevated hs-cTnT ( ≥ 14 ng/L) was observed in 64.0% (n = 32) of patients. Above findings showed there were no statistically significant differences between the two groups in term of baseline characteristics and echocardiographic findings and mortality, however hs-cTnT and WBC were high in non-survivor group significantly.
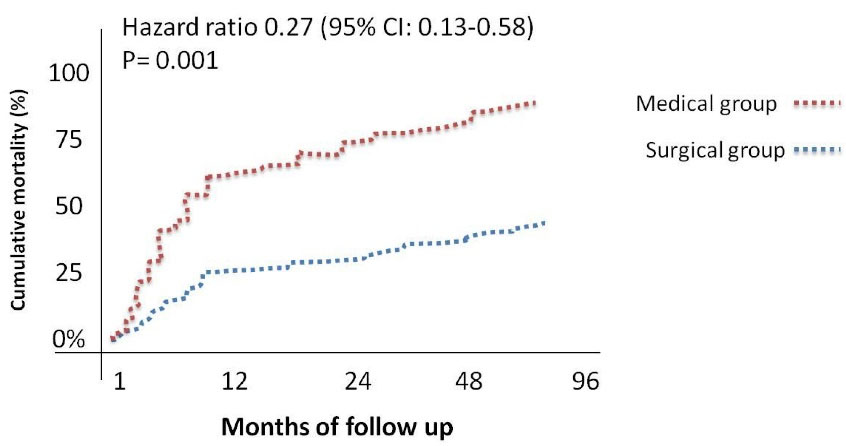
Figure 2.
Kaplan-meier analysis of cumulative mortality among patients in the medical and surgical groups
.
Kaplan-meier analysis of cumulative mortality among patients in the medical and surgical groups
Table 2.
Association of baseline characteristics, first laboratory investigation, echocardiographic findings and surgical approach and survival of the patients
|
Variable
|
Total (N=50)
|
Non Survivor (n=29)
|
Survivor (n=21)
|
P
-value
|
| Gender (Male) |
29 (58%) |
14 (48.3%) |
15 (71.4%) |
0.147 |
| Age |
57.2 ± 16.16 |
62.73 ± 17.74 |
49.4 ± 10.25 |
0.056 |
| Limb paralysis |
4 (8%) |
3 (10.3%) |
1 (4.8%) |
0.556 |
| syncope |
9 (18%) |
6 (20.7%) |
3 (14.3%) |
0.451 |
| SBP (mmHg) |
138.5 ± 27.5 |
140.69 ± 25.6 |
135.52 ± 30.4 |
0.780 |
| Heart rate (Beats/min) |
84.3 ± 2087 |
85.1 ± 23.62 |
83.38 ± 16.87 |
0.966 |
| History of CAD* |
11 (22%) |
9 (31%) |
2 (9.5%) |
0.071 |
| History of HTN* |
31 (62%) |
19 (65.5%) |
12 (57.1%) |
0.817 |
| History of CVA* |
3 (6%) |
2 (6.9%) |
1 (4.8%) |
0.694 |
| History of CKD* |
1 (2%) |
0 (0%) |
1 (4.8%) |
0.417 |
| hs Troponin T level (ng/dl) |
20.52 (9-100) |
31.99 (16.3-125.8) |
11.3 (5.6-40) |
0.005 |
| D-dimer level (ng/dl) |
4.54 (1.2-106) |
4.72 (1.7-7.7) |
1.7 (0.6-19.6) |
0.771 |
| White blood cell count ( × 10³) |
10.8 (9.3-13.3) |
11.5 (9.7-13.7) |
9.4 (8.7-13) |
0.018 |
| Platelet count ( × 10³) |
173 (131.2-225.4) |
152.1 (113-224) |
197 (159.3-228.7) |
0.771 |
| Hemoglobin (mg/dl) |
12.9 ± 2.25 |
12.54 ± 2.37 |
13.43 ± 2.01 |
0.241 |
| Creatinine (mg/dl) |
1 (0.8-1.5) |
1.03 (0.8-1.6) |
1 (0.8-1.25) |
0.867 |
| Ejection fraction (%) |
53.2 ± 10.3 |
53 ± 10.26 |
54.4 ± 10.4 |
0.708 |
| Moderate AI ≤ |
36 (73.5%) |
22 (75.9%) |
14 (70%) |
0.588 |
| Ascending aorta diameter (mm) |
55.4 ± 14.5 |
54.4 ± 15.06 |
56.8 ± 13.9 |
0.431 |
| Pericardial effusion |
20 (40.8%) |
12 (41.4%) |
8 (40%) |
0.855 |
| Medical treatment |
19 (38%) |
17 (58.6) |
2 (9.5%) |
0.013 |
| Surgical approach |
31 (62%) |
12 (44.4%) |
19 (90.5%) |
0.001 |
*SBP, Systolic blood pressure; CAD, Coronary artery disease; HTN, Hypertension; CVA, Cerebrovascular arrest; CKD, Chronic kidney disease; AI, Aortic insufficiency.
Multivariable analysis showed only an increase in hs-cTnT levels was suggested as a predictor of mortality (95% CI: 1.06–1.38; HR = 1.21; P= 0.005), so that for every 100 units increase, patients were 21% more likely to have mortality in long term. Also, performing surgical treatment for aortic dissection was determined as the independent predictor of surviving, so that death was 74.6% less than those who received medical treatment (95% CI: 0.13–0.58; HR = 0.27; P= 0.001) (Figure 3).
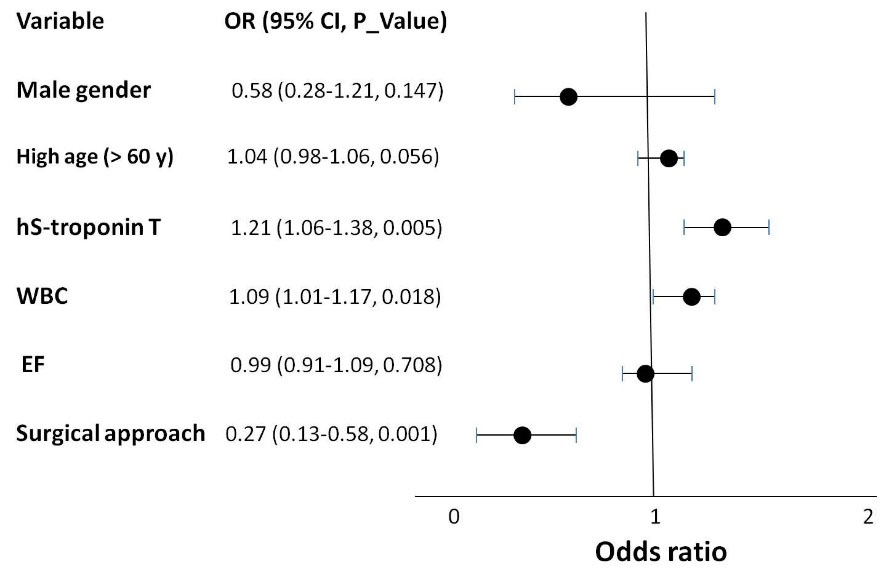
Figure 3.
Forest plot of the odds ratio for 3 years mortality of acute aortic dissection type A. High hs-troponin T levels significantly increased long-term mortality. Also, long-term mortality was significantly less in the surgical approach
.
Forest plot of the odds ratio for 3 years mortality of acute aortic dissection type A. High hs-troponin T levels significantly increased long-term mortality. Also, long-term mortality was significantly less in the surgical approach
Discussion
Therefore, AAD is a highly lethal medical or surgical emergency. However, to date, there is no clinical risk stratification model for patients with AAD
4
and AAD is associated with a great deal of forgetfulness due to the lack of specific clinical symptoms.
5
After clinical suspicion, its diagnosis is made by echocardiography or CT angiography. At present, none of the laboratory findings play with high sensitivity and specificity a role in the diagnosis and prognosis of patients.
6
However, our study shows that hs-cTnT, WBC and NLR are significantly associated with long-term mortality in these patients. Other studies have shown prognostic role of D-dimer, C reactive protein (CRP), matrix metalloproteinases, smooth muscle myosin heavy chain, and soluble elastin fragments in AAD type A.
7
Although the role of troponins in acute vascular syndromes including acute coronary syndromes and acute pulmonary embolism has been confirmed as a prognostic factor, its role in acute aortic dissection has not yet been well established.
8
Troponin levels as seen in this study can be increased between 23% and 33% of patients with AAD type A which this condition increases the likelihood of misdiagnosis and missing of ADA. Mechanisms of increased Troponin levels in dissection include ischemia due to severe hypotension, ischemia due to severe aortic valve insufficiency, covering of the coronary artery by the intimal flap, and sometimes extension of the intimal flap into the coronary arteries.
8
Most previous studies have focused more on increasing hs-cTn after surgery and its association with increased mortality,
9
while surgery itself can increase hs-cTn and therefore have false results. Therefore, in this study, we included patients undergoing both medical and surgical treatment and examined preoperative hs-cTnT levels.
10
Unlike to our study, the above studies and several other studies have also evaluated in-hospital and short-term mortality that increasing of hs-cTnT levels significantly increases mortality.
11
However, the results of large sample of single center in China showed that an increase in troponin was not associated with long-term mortality of AAD. However, in the above study, hs-cTnI was examined, while in our study, hs-cTnT was considered.
12
Except for the above study and our study; No other study has evaluated the association between long-term mortality and hs-cTnT.
The value of biomarkers depends on their clinical availability, and their cost-effectiveness is a precondition for their use in the clinical routine test.
13
The utility of hs-cTnT measurement as a routine test for risk stratification in patients with AAD cannot be established by this single-center study and more large studies are required.
Conclusion
The results of present study showed the level of hs-cTnT has a potential utility for predict of long-term mortality in patients with AAD type A.
Acknowledgements
None.
Competing Interests
The authors declare that they have not competing financial interests or personal relationships that could have influenced the work reported in this paper.
Ethical Approval
This study was approved by ethics committee of Tehran heart center with the ethical code of 8751.
Funding
None.
References
- Khederlou H, Jenab Y. Spontaneous aortic dissection type a as the first manifestation of autosomal dominant polycystic kidney disease: a case report. Int J Case Rep Short Rev 2021; 16(7):5-8. doi: 10.37871/ijcrsr.id94 [Crossref] [ Google Scholar]
- Ranasinghe AM, Bonser RS. Biomarkers in acute aortic dissection and other aortic syndromes. J Am Coll Cardiol 2010; 56(19):1535-41. doi: 10.1016/j.jacc.2010.01.076 [Crossref] [ Google Scholar]
- Karakoyun S, Gürsoy MO, Akgün T, Öcal L, Kalçık M, Yesin M. Neutrophil-lymphocyte ratio may predict in-hospital mortality in patients with acute type A aortic dissection. Herz 2015; 40(4):716-21. doi: 10.1007/s00059-014-4121-2 [Crossref] [ Google Scholar]
- Pape LA, Awais M, Woznicki EM, Suzuki T, Trimarchi S, Evangelista A. Presentation, diagnosis, and outcomes of acute aortic dissection: 17-year trends from the International Registry of Acute Aortic Dissection. J Am Coll Cardiol 2015; 66(4):350-8. doi: 10.1016/j.jacc.2015.05.029 [Crossref] [ Google Scholar]
- Nienaber CA, Clough RE, Sakalihasan N, Suzuki T, Gibbs R, Mussa F. Aortic dissection. Nat Rev Dis Primers 2016; 2:16053. doi: 10.1038/nrdp.2016.53 [Crossref] [ Google Scholar]
- Bossone E, Czerny M, Lerakis S, Rodríguez-Palomares J, Kukar N, Ranieri B. Imaging and biomarkers in acute aortic syndromes: diagnostic and prognostic implications. Curr Probl Cardiol 2021; 46(3):100654. doi: 10.1016/j.cpcardiol.2020.100654 [Crossref] [ Google Scholar]
- Mir MA. Aortic dissection--in pursuit of a serum marker. Am J Emerg Med 2008; 26(8):942-5. doi: 10.1016/j.ajem.2007.12.012 [Crossref] [ Google Scholar]
- Vrsalovic M. Prognostic effect of cardiac troponin elevation in acute aortic dissection: a meta-analysis. Int J Cardiol 2016; 214:277-8. doi: 10.1016/j.ijcard.2016.03.230 [Crossref] [ Google Scholar]
- Bojan M, Peperstraete H, Lilot M, Vicca S, Pouard P, Vouhé P. Early elevation of cardiac troponin I is predictive of short-term outcome in neonates and infants with coronary anomalies or reduced ventricular mass undergoing cardiac surgery. J Thorac Cardiovasc Surg 2012; 144(6):1436-44. doi: 10.1016/j.jtcvs.2012.05.034 [Crossref] [ Google Scholar]
- Bottio T, Vida V, Padalino M, Gerosa G, Stellin G. Early and long-term prognostic value of troponin-I after cardiac surgery in newborns and children. Eur J Cardiothorac Surg 2006; 30(2):250-5. doi: 10.1016/j.ejcts.2006.05.001 [Crossref] [ Google Scholar]
- Vrsalovic M, Zeljkovic I, Presecki AV, Pintaric H, Kruslin B. C-reactive protein, not cardiac troponin T, improves risk prediction in hypertensives with type A aortic dissection. Blood Press 2015; 24(4):212-6. doi: 10.3109/08037051.2015.1025607 [Crossref] [ Google Scholar]
- Gong M, Wu Z, Guan X, Jiang W, Zhang H. Comparison of prognostic ability of perioperative myocardial biomarkers in acute type A aortic dissection. Medicine (Baltimore) 2019; 98(43):e17023. doi: 10.1097/md.0000000000017023 [Crossref] [ Google Scholar]
- Mohamed SA, Misfeld M, Richardt D, Sievers HH. Identification of candidate biomarkers of acute aortic dissection. Recent Pat DNA Gene Seq 2008; 2(1):61-5. doi: 10.2174/187221508783406567 [Crossref] [ Google Scholar]