J Cardiovasc Thorac Res. 17(1):20-26.
doi: 10.34172/jcvtr.33167
Original Article
Baseline characteristics and seven-year follow-up of patients with coronary slow flow: A cohort study in northeastern Iran
Farima Farsi Conceptualization, Investigation, Methodology, Writing – original draft, 1 
Negar Morovatdar Data curation, Formal analysis, Methodology, Validation, Visualization, 2
Ali Eshraghi Conceptualization, Project administration, Resources, Supervision, Writing – review & editing, 3, * 
Author information:
1Obesity and Eating Habits Research Center, Endocrinology and Metabolism Clinical Sciences Institute, Tehran University of Medical Sciences, Tehran, Iran
2Clinical Research Development Unit, Faculty of Medicine, Mashhad University of Medical Sciences, Mashhad, Iran
3Department of Cardiology, Faculty of Medicine, Mashhad University of Medical Sciences, Mashhad, Iran
Abstract
Introduction:
An angiographic finding known as "coronary slow flow phenomenon" (CSFP) occurs when there is no discernible stenosis but the contrast flow is slower than usual. Although the prognosis for the majority of CSFP cases is favorable, frequent angina significantly lowers their quality of life. Therefore, this study aimed to explore the potential contributing risk factors and prognostic implications of CSFP on long-term cardiovascular outcomes.
Methods:
This retrospective, cohort study was conducted between years 2014-2022 and included a total of 65 CSFP patients and 65 controls with normal coronary flow, as evidenced by coronary angiography. These two groups were examined in terms of future cardiovascular consequences due to this phenomenon, baseline demographic characteristics, and laboratory findings. A P value<0.05 was considered significant.
Results:
In this study 130 people including 73 men and 57 women, who because of the typical chest pain and at least a noninvasive test took angiography, were explored. The median triglyceride (200.80±48.51 vs 131.79±34.22, P<0.001), total cholesterol (189.46±10.84 vs 103.43±8.13, P<0.001), and low-density lipoprotein (153.28±34.28 vs 103.34±19.70, P=0.01) were significantly higher in the affected people. During clinical follow-up, a higher number of major adverse cardiac events (8.97±2.95 vs 4.52±2.12, P<0.001) was observed in the CSFP cases. Moreover, a one-unit increase in body mass index raised the probability of adverse cardiac events by 0.912 in CSFP cases.
Conclusion:
Our research indicated that individuals with CSFP were more likely to develop cardiac events including unstable angina. Furthermore, obesity and dyslipidemia could provoke this phenomenon.
Keywords: Adverse cardiac events, Coronary slow flow, Dyslipidemia
Copyright and License Information
© 2025 The Author(s).
This is an open access article distributed under the terms of the Creative Commons Attribution License (
http://creativecommons.org/licenses/by/4.0/), which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited.
Funding Statement
Authors of this manuscript received no financial support for the research, authorship, and publication of the article.
Introduction
The term “coronary slow flow phenomenon” (CSFP) or syndrome Y refers to a condition where coronary angiography shows no significant lesion in the epicardial coronary arteries but with delayed blood perfusion. It is not associated with thrombolytic treatment, coronary angioplasty, arterial spasm, coronary dilatation or stenosis, cardiomyopathy, significant valvular heart disease, decompensated heart failure, and specific connective tissue disorders of the coronary microvasculature.1 Among patients who underwent coronary angiography due to chest pain, 1%-7% of them have confirmed CSFP. Additionally, four percent of patients with unstable angina also had CSFP. Clinical signs and symptoms of coronary atherosclerotic disease are comparable in CSFP.2,3 Repetitive typical chest pain is the most common symptom observed in patients with CSFP.4 Although the prognosis for the majority of CSFP cases is favorable,5 frequent angina significantly lowers the quality of life. Furthermore, this phenomenon could result in recurrent hospitalization, repeated coronary angiography, myocardial ischemia, and ultimately acute coronary syndrome (ACS). Young male patients and smokers are more likely to experience this condition.3,6,7 Other risk factors such as hypertension (HTN),8, low levels of high-density lipoprotein cholesterol (HDL-C),9 diabetes mellitus (DM), and high body mass index (BMI) have been suggested to correlate with this condition.10 The exact mechanism of CSFP is still unknown, however, its pathophysiology has been linked to several variables including microvascular abnormalities, inflammation, structural, and functional abnormalities of blood cells, vascular endothelial dysfunction, atherosclerosis, and metabolic disorders.11 Patients who were histologically investigated had the following findings: myofibrillar hypertrophy, inflammation of the wall of microvessels, endothelial damage, and arterial stenosis.3,12 CSFP currently lacks a definitive treatment due to its unclear mechanism. In the clinic, empirical treatment mostly consists of the following elements: management of cardiovascular risk factors, such as diabetes, hyperlipidemia, and hypertension,13 antiplatelet medications,14 calcium channel blockers, nitrate medications,13 and beta blockers.15
One of the diagnostic methods is the stress exercise test, however, it could not detect all patients with CSFP.16 Another way to recognize this phenomenon is coronary angiography, which can determine the blood flow rate in myocardial arteries quantitatively and has been used extensively to assess acute myocardial infarction.
Diagnosis of the cardiac source of chest pain in patients affected by CSFP has been challenging for cardiologists since their coronary angiography is nearly normal. Due to the unclear mechanism of this phenomenon, there is no definite cure, nor has the syndrome been extensively studied whether this angiographic finding is related to a pathological process in the coronary artery with an unfavorable prognosis for cardiovascular events or is natural. Considering that the most common manifestation of this phenomenon is frequent chest pain, it could have a significant impact on a person’s quality of life; therefore, we aimed to follow up patients who were referred to our clinic due to typical chest pain, underwent coronary angiography, and were diagnosed with CSFP. Furthermore, we examined the function of clinical traits in CSFP patients and served as a guide for future research into the possible mechanisms underlying CSFP.
Materials and Methods
Coronary angiography
Y syndrome is only diagnosed in patients whose angiography is relatively normal and is not influenced by atherosclerotic coronary artery disease. Intravascular ultrasound revealed that a large number of people whose angiogram was normal had extensive atherosclerotic heart disease.17 The researchers use two approaches to define the slow flow of contrast matter in angiography:
simple
-
a) Thrombolysis in myocardial infarction (TIMI) flow grade: It is a semi-quantitative method that grades contrast material flow in epicardial vessels from TIMI-0 (no flow) to TIMI-3 (natural flow). TIMI-2 is considered to be turbidity at the end of the vascular bed. This method has been also used to detect the non-flow phenomenon.18
-
b) TIMI frame count: This approach was first devised by Gibson et al19, and is a quantitative method in which the number of frames required for the opacification of the vascular bed is calculated. The reference value of 23 ± 3 frames is considered, so some researchers estimate values higher than that to be slow flow 17 while others take into account the required number of frames greater than two standard deviations of reference value as CSFP.7 It is worth noting that studies using this method have reported an average of more than 50 frames as CSFP.18
Baseline definition and measurements
In the current study, having a fasting blood sugar (FBS) of at least 126 mg/dl twice in addition to clinical symptoms (weight loss, polyuria, and polydipsia), a Hemoglobin A1C (HbA1C) of at least 6.4, or a prior history of the illness were all considered indicators of DM. A normal lipid profile was defined as low-density lipoprotein (LDL-C) < 100 mg/dl, HDL-C ≥ 50 mg/dl for women HDL-C ≥ 40 mg/dl for men, and total cholesterol < 200 mg/dl. Hypertension was described as systolic blood pressure (SBP) ≥ 140 mmHg and/or diastolic blood pressure (DBP) ≥ 90 mmHg.
Based on the angiographic findings of the patients, CSFP was defined as delayed distal opacification (TIMI-flow 2) in at least one epicardial vessel (Table 1). For additional insight into the coronary angiographic findings, please refer to Supplementary files 1-4.
Table 1.
Proposed criteria for defining CSFP
|
Angiographic evidence of the CSFP, defined by:
|
Exclusion of secondary causes of the CSFP, including:
|
simple
-
• No evidence of obstructive epicardial CAD (i.e. No angiographic lesions ≥ 40%)
|
|
simple
-
• Delayed distal vessel contrast opacification as evidenced by either:
|
|
simple
-
a. TIMI-2 flow (i.e. requiring ≥ 3 beats to opacify the vessel), or
|
|
simple
-
b. Corrected TIMI frame count ≥ 27 frames (images acquires < 30 frames/s)
|
simple
-
• Exogenous vasoconstrictor administration (e.g., cocaine)
|
Abbreviations: CSFP, coronary slow flow phenomenon; CAD, coronary artery disease; TIMI, thrombolysis in myocardial infarction. Criteria adapted from Nurkalem et al. (2008).12
Design and population of the study
This was a seven-year cohort study, conducted in Imam Reza Teaching Hospital, a referral hospital in Iran. The protocol of the study was approved by the research ethics committee of Mashhad University of Medical Sciences (ethical code: IR.MUMS.MEDICAL.REC.1401.086). In total, 65 consecutive patients with CSFP and 65 normal controls were enrolled between March 2012 and February 2016 and were followed for 84 months ± 14 days (Figure 1). The exclusion criteria were as follows: moderate to severe valvular heart disease, heart failure (ejection fraction less than 40%), acute or chronic inflammatory disorders, renal disorders (protein-losing nephropathy with Albumin-creatinine ratio (ACR) < 300 and/or glomerular filtration rate (GFR) < 90 ml/min), liver disorders, coronary ectasia in angiography, history of myocardial infarction (MI) and/or primary cutaneous intervention (PCI), non-sinus rhythm in electrocardiogram (ECG), congenital heart disease, infection or having fever, chronic obstructive pulmonary disease (COPD), antioxidants consumption, and thrombolytic treatment. All patients provided informed consent and the study was conducted in accordance with the ethical principles described by the declaration of Helsinki.
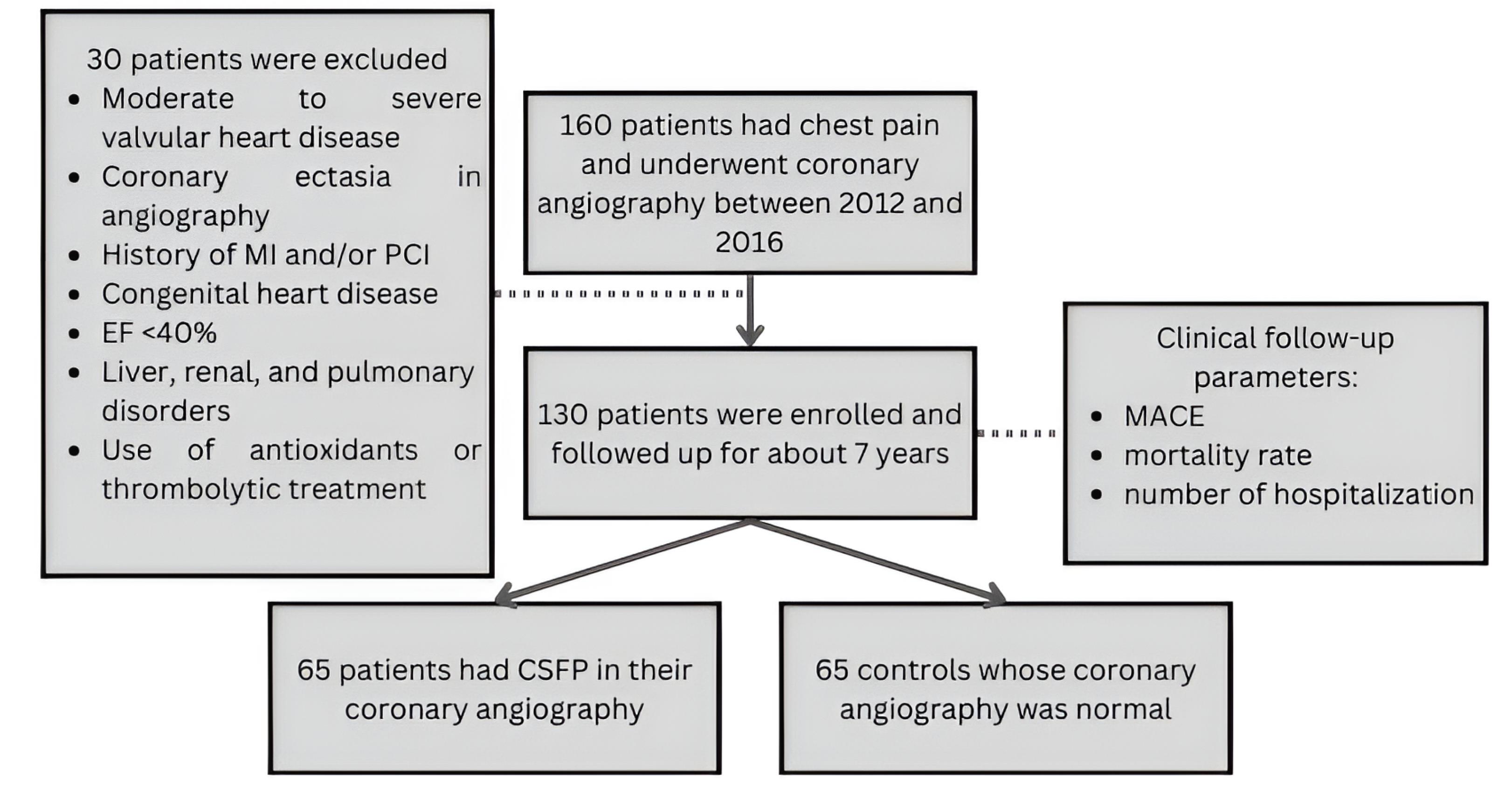
Figure 1.
Flowchart of enrolment of the study participants, abbreviations: MI, myocardial infarction, PCI, percutaneous coronary intervention, EF, ejection fraction, MACE, major adverse cardiac events, CSFP, coronary slow flow phenomenon
.
Flowchart of enrolment of the study participants, abbreviations: MI, myocardial infarction, PCI, percutaneous coronary intervention, EF, ejection fraction, MACE, major adverse cardiac events, CSFP, coronary slow flow phenomenon
Follow-up
In this retrospective cohort study 130 patients who had typical chest pain and a positive result of a non-invasive test such as an exercise stress test or an indication for performing angiography including a strong family history of cardiovascular problems, old age or marked functional limitation, etc., and underwent angiography between March 2012 and February 2016 were enrolled and followed up for 84 months ± 14 days by maintaining consistent communication every year to prevent loss of communication. These subjects were followed for seven years for mortality rate, number of hospitalizations, and major adverse cardiac event (MACE, need for or performing repeated interventions such as PCI and coronary artery bypass graft, acute coronary syndrome) which were performed while explaining the study and assuring appropriate use of the information. Furthermore, demographic characteristics, angiographic findings, and laboratory parameters were explored using their medical records at the hospital and physical examination performed on arrival.
Statistical analysis
The final data were analyzed using IBM SPSS Statistics for Windows, Version 23 (IBM Corp., Armonk, NY, USA). The data were described using the statistical indices mean, frequency, and standard deviation. Depending on the normality of data distribution the Student’s t-test was used to investigate the quantitative variables, while the qualitative variables were analyzed using the chi-squared test. To determine the relationship between MetS and the variables, we used Logistic Regression. The significance level was considered as P < 0.05 for all the comparisons.
Results
In this retrospective cohort study, 130 patients were enrolled and clinically followed up for 84 months ± 14 days. Among the studied population, sixty-five cases had CSFP in their angiograms, and an equal number did not. Of these, 73 were men (56.15%) and 57 were women (43.85%).
Demographic indices in two groups with CSFP and normal group
According to Table 2, the number of diabetics, people with abnormal lipid profile and mean BMI in the CSFP group were 67.69% (vs. 47.69%, P = 0.03), 52.31% (vs. 47.69%, P = 0.03), and 27.18 ± 1.18 (vs 24.98 ± 1.44, P > 0.001), respectively. There was no significant difference in age (P = 0.47), gender (P = 0.72), smoking (P = 0.59), and systolic blood pressure (P = 0.55).
Table 2.
Comparison of demographic indices between two groups with and without CSFP
|
Demographic characteristics
|
Total
(n=130)
|
CSFP group
(n=65)
|
Normal group
(n=65)
|
P
value
|
| Age (years) |
63.18 ± 11.07a |
62.26 ± 10.68a |
64.09 ± 11.45a |
0.47 |
| Gender |
|
|
|
0.72 |
| Female |
57 (43.85%) |
27 (41.53%) |
30 (46.15%) |
| Male |
73 (56.15%) |
38 (58.46%) |
35 (53.84%) |
| SBP (mmHg) |
140.88 ± 9.96a |
141.4 ± 8.02a |
140.37 ± 11.63a |
0.55 |
| DM |
75 (57.7%) |
44 (67.69%) |
31 (47.69%) |
< 0.03 |
| Smoking |
48 (36.92%) |
22 (33.85%) |
26 (40.00%) |
0.59 |
| Abnormal lipid profile |
65 (50%) |
34 (52.31%) |
31 (47.69%) |
0.03 |
| BMI |
26.08 ± 1.71a |
27.18 ± 1.18a |
24.98 ± 1.44a |
< 0.001 |
Values are counts (percentages) unless stated otherwise, a Mean ± standard deviation. Percentages are estimated within each group with and without CSFP. Abbreviations: CSFP, coronary slow flow phenomenon, SBP, systolic blood pressure, DM, diabetes mellitus, BMI, body mass index.
Laboratory data in patients with and without CSFP
In terms of laboratory parameters, mean monocyte count, hemoglobin, blood glucose, total cholesterol, triglyceride, and LDL-C in the CSFP group were 0.39 ± 0.08 (vs. 0.33 ± 0.05, P = 0.01), 13.36 ± 1.96 (vs. 12.69 ± 1.72, P = 0.04), 103.69 ± 7.12 (vs. 90.43 ± 5.51, P > 0.001), 10.69 ± 10.64 (vs. 103.43 ± 8.13 vs. P > 0.001), 200.80 ± 48.51 (vs. 131.79 ± 34.22, P > 0.001 and 153.28 ± 34.28 (vs. 103.34 ± 19.70, P = 0.01) (Table 3). All of the CSFP patients had significantly higher amount of BMI, blood sugar, and total cholesterol than the normal group.
Table 3.
Comparison of laboratory parameters between two groups with and without CSFP
|
Laboratory data
|
Total (n=130)
|
CSFP group (n=65)
|
Normal group (n=65)
|
P
value
|
| WBC count (109/L) |
8.18 ± 1.56 |
8.04 ± 1.54 |
8.37 ± 1.57 |
0.32 |
| Monocyte count (109/L) |
0.36 ± 0.13 |
0.39 ± 0.08 |
0.33 ± 0.05 |
0.01 |
| RBC count (109/L) |
4.58 ± 0.35 |
4.63 ± 0.37 |
4.52 ± 0.33 |
0.76 |
| Hb (g/dl) |
13.03 ± 1.87 |
13.36 ± 1.96 |
12.69 ± 1.72 |
0.04 |
| RDW (%) |
12.23 ± 1.63 |
12.01 ± 1.63 |
12.44 ± 1.62 |
0.13 |
| BS (mg/dl) |
97.06 ± 9.19 |
103.69 ± 7.12 |
90.43 ± 5.51 |
< 0.001 |
| Total cholesterol (mg/dl) |
146.45 ± 44.20 |
189.46 ± 10.64 |
103.43 ± 8.13 |
< 0.001 |
| HDL-C (mg/dl) |
47.22 ± 6.39 |
42.53 ± 6.56 |
51.91 ± 6.23 |
0.76 |
| LDL-C (mg/dl) |
128.31 ± 26.99 |
153.28 ± 34.28 |
103.34 ± 19.70 |
0.01 |
| TG (mg/dl) |
166.30 ± 41.37 |
200.80 ± 48.51 |
131.79 ± 34.22 |
< 0.001 |
| ALT (IU/L) |
25.82 ± 9.36 |
27.32 ± 10.11 |
24.10 ± 8.36 |
0.06 |
| AST (IU/L) |
30.92 ± 10.96 |
31.72 ± 11.50 |
30.12 ± 10.41 |
0.40 |
| Creatinine (mg/dl) |
1.09 ± 0.36 |
1.11 ± 0.36 |
1.05 ± 0.36 |
0.33 |
Values are Mean ± standard deviation. Abbreviations: CSFP, coronary slow flow phenomenon, WBC, white blood cell, RBC, red blood cell, Hb, hemoglobin, RDW, red cell distribution width, BS, blood sugar, HDL-C, high-density lipoprotein cholesterol, LDL-C, low-density lipoprotein cholesterol, TG, triglycerides, ALT, alanine aminotransferase, AST, aspartate aminotransferase.
On binary logistic regression analysis on all subjects (Table 4), we observed that the higher BMI of the patient was most significantly associated with the occurrence of CSFP (odds ratio [OR] = 6.680 [3.250-13.730], P < 0.001). In addition to that, high BS (OR = 1.736 [1.412-2.135], P < 0.001), abnormal lipid profile (OR = 2.949 [1.440-6.038], P = 0.003), high total cholesterol (OR = 2.442 [1.853-3.031], P < 0.001, increased LDL-C (OR = 1.541 [1.012-2.070], P < 0.001), and TG (OR = 1.328 [1.006-1.650], P = 0.043) were associated with higher odds of CSFP.
Table 4.
Binary logistic regression analysis for prediction of CSFP
|
Variable
|
OR
|
95% CI for EXP (B)
|
P
value
|
|
Lower
|
Upper
|
| DM |
0.435 |
0.213 |
0.887 |
0.022 |
| Abnormal lipid profile |
2.949 |
1.440 |
6.038 |
0.003 |
| BMI |
6.680 |
3.250 |
13.730 |
< 0.001 |
| Monocyte count |
0.573 |
0.130 |
0.998 |
0.064 |
| Hb |
0.876 |
0.143 |
1.609 |
0.544 |
| BS |
1.736 |
1.412 |
2.135 |
< 0.001 |
| Total cholesterol |
2.442 |
1.853 |
3.031 |
< 0.001 |
| LDL-C |
1.541 |
1.012 |
2.070 |
< 0.001 |
| TG |
1.328 |
1.006 |
1.650 |
0.043 |
Abbreviation: DM, diabetes mellitus, BMI, body mass index, Hb, hemoglobin, BS, blood sugar, LDL-C, low-density lipoprotein cholesterol, TG, triglycerides.
Follow-up data of the two groups with and without CSFP
As shown in Table 5, the mean number of hospitalizations, ACS, stable angina, and MACE in the CSFP group was 1.50 ± 2.05 (vs. 1.10 ± 1.89 and P = 0.03), 1.75 ± 1.2 (vs. 0.89 ± 0.95 and P > 0.001), 0.93 ± 5.45 (vs. 0.78 ± 2.78 and P > 0.001), 2.95 ± 8.97 (vs. 4.52 ± 2.12 vs. P > 0.001), respectively. The number of deaths during these seven years of follow-up war 6 in CSFP patients (vs. 0, P = 0.03), which was not cancer- or trauma-related. Furthermore, the CSFP cases had lower performance levels than the normal group (P < 0.001).
Table 5.
Seven-year follow-up data of the two groups with and without CSFP
|
Follow-up data
|
Total
(n=130)
|
CSFP group
(n=65)
|
Normal group
(n=65)
|
P
value
|
| Hospitalization |
1.96 ± 1.33 |
2.05 ± 1.50 |
1.89 ± 1.10 |
0.03 |
| MACE |
6.75 ± 3.40 |
8.97 ± 2.95 |
4.52 ± 2.12 |
< 0.001 |
| Death |
6a |
6a |
0a |
0.03 |
| ACS |
1.35 ± 1.13 |
1.75 ± 1.20 |
0.95 ± 0.89 |
< 0.001 |
| Stable angina |
4.12 ± 1.59 |
5.45 ± 0.93 |
2.78 ± 0.78 |
< 0.001 |
| NYHA functional class |
|
|
|
< 0.001 |
| Class I |
|
5 (7.69%)a |
30 (46.15%)a |
| Class II |
|
37 (59.92%)a |
35 (53.85%)a |
| Class III |
|
17 (26.15%)a |
0 (0.00%)a |
| Class IV |
|
6 (9.23%)a |
0 (0.00%)a |
Values are Mean ± standard deviation unless stated otherwise, a number (percentage). Abbreviations: CSFP, coronary slow flow phenomenon, MACE, major adverse cardiac events, ACS, acute coronary syndrome, NYHA, New York Heart Association.
As illustrated in Figure 2, by increasing blood glucose, body mass index, and total cholesterol, MACE level increases in a relatively linear manner. Linear regression test was used to create a model that could exactly determine a linear relationship between MACE as the dependent variable and BS, total cholesterol, and BMI. A one-unit increase in BS, total cholesterol, and BMI raised the MACE rate by 0.293 (0.293 × BS-21.731 = MACE, P < 0.001), 0.053 (0.053 × total cholesterol-0.930 = MACE, P < 0.001), and 0.912 (0.912 × BMI-17.055 = MACE, P < 0.001), respectively.
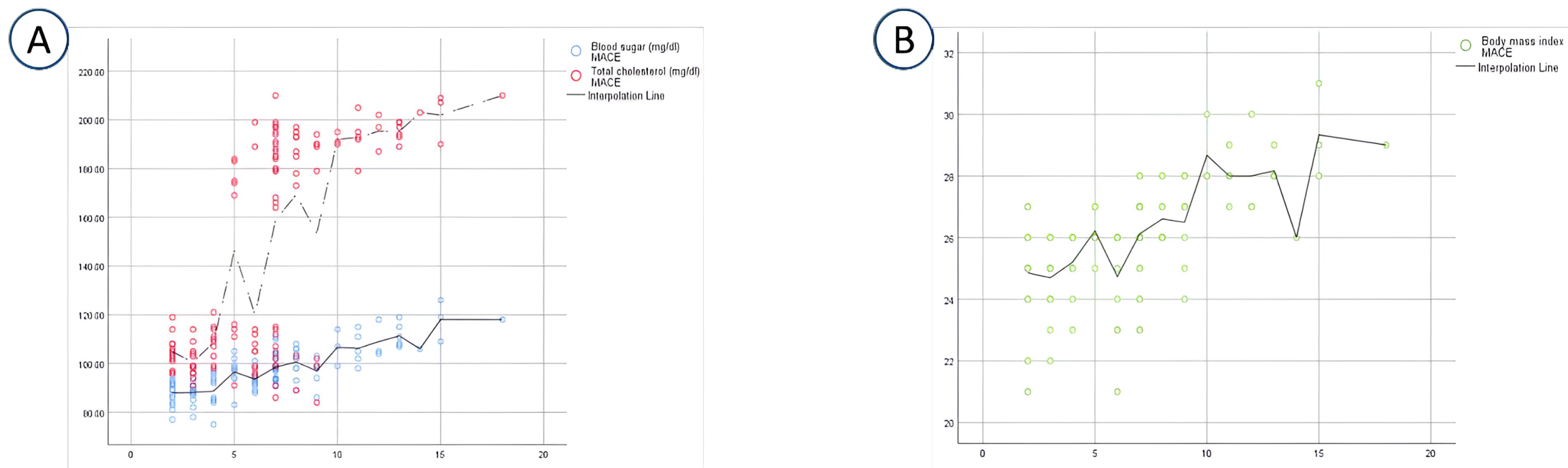
Figure 2.
Correlation of Blood sugar, total cholesterol (A), body mass index (B), and major adverse cardiac events in the study population
.
Correlation of Blood sugar, total cholesterol (A), body mass index (B), and major adverse cardiac events in the study population
Discussion
CSFP is a relatively common finding in angiograms of people who undergo angiography due to cardiac chest pain and a disruptive result of a noninvasive test.
In the study of Wang et al CSFP had similar clinical manifestations of coronary atherosclerosis disease, which is consistent with our findings. Based on our study, such as that of John Beltreem et al,6 the MACE rate and the frequency of hospitalization and deaths related to or without cardiovascular disorders were significantly higher in the CSFP group, which contradicted the results of Mosseri et al 3 and Sadamusta et al,20 in which it was noted that this phenomenon had a good prognosis, however, due to the association of this phenomenon with adverse cardiovascular events, the necessity of clinical follow-up of these patients was emphasized. In a study conducted by Sadr Ameli et al the most common complaint of patients with CSFP was recurrent non-typical chest pain. In their study, a significant number of patients required re-angiography, and one-sixth of them had significant narrowing in their coronary arteries. 21 According to our study, a significant number of patients reported a history consistent with acute coronary syndrome. Mosseri et al3 discovered that recurrent chest pain was the most typical way that this phenomenon manifested itself, and the majority of patients in our study had a history of recurrent cardiac chest pain. In the study of Alvarez et al it was also noted that CSFP should be considered as a separate differential diagnosis for acute chest pain.22 The level of performance of the CSFP cases according to NYHA classification was in higher stages than the normal group.
In this study, the risk factors that could according to the previous studies predict the occurrence of this phenomenon were also evaluated. Wang et al concluded that CSFP was more common in males and smokers 2, and Weferling et al noted in their research that the only difference in basic characteristics of those with and without this phenomenon was smoking 23 but in our study there was no significant relationship between smoking and male gender and this phenomenon. In the study of Huang et al and Afsin et al it has been suggested that metabolic syndrome and atherosclerotic diseases could be predictors of this phenomenon.11,24 According to our study, the number of people with diabetes, abnormal lipid profile, and the mean BMI in the CSFP group were significantly higher than the normal group. Furthermore, Zavala-Alarcon et al also and Seyyed Mohammadzad et al mentioned high BMI and diabetes as risk factors for this phenomenon.10,25 In the study of Pekdemir et al disseminated calcification, and atherosclerosis were also proposed as the underlying mechanism of this phenomenon.26 Moreover, Binak et al found a significant relationship between blood sugar levels and susceptibility to this phenomenon.27 There was no significant difference in age (P value = 0.479), gender (P value = 0.72), smoking (P value = 0.59), and systolic blood pressure (P = 0.55). Unlike the study of Alarcon et al and Sezgin et al which identified high blood pressure and low HDL-c as predisposing factors to this syndrome,10,28 in our study there was no significant relationship between systolic blood pressure and HDL cholesterol and this phenomenon. In another study performed on CSFP patients and control group, there was no difference in blood pressure level.29
In the study conducted by Hockey Simsek et al,15 the use of Nebivolol (a Beta-blocker) was found to be effective in preventing from this phenomenon, especially from related arrhythmias, but in our study no difference was observed in the use of beta-receptor blockers between the CSFP and normal groups. Xia et al have suggested platelet inhibitors for coronary artery dilation,14 but accordingly in our study, its beneficial effect in preventing CSFP was not affected in any way by its use between the two groups with and without this phenomenon. Also, unlike the study that Zavala Alarcon and his colleagues had conducted on calcium receptor inhibitors and its effect on prevention of this phenomenon,10 its use did not differ significantly between the two groups in our study, and as a result, it had no detrimental effect on CSFP prevention.
In terms of laboratory parameters, the mean monocyte count, hemoglobin, blood sugar, total cholesterol, triglyceride, and LDL-c in CSFP cases were higher than controls. There was no significant difference in the type and amount of medications used between the normal and CSFP subjects. Therefore, no specific treatment could be suggested that can be effective in preventing the occurrence of this phenomenon.
Conclusion
According to our study, this phenomenon could affect the quality of life and be a predictor of adverse cardiovascular events. Therefore, the need for clinical follow-up of patients to understanding the underlying pathophysiology of this phenomenon and providing suitable treatment is emphasized.
Competing Interests
The authors declare that there is no conflict of interest.
Ethical Approval
The research ethics committee at Mashhad University of Medical Sciences granted approval for the study protocol, assigned the ethical code IR.MUMS.MEDICAL.REC.1401.086. Written informed consent was obtained from the patients to publish this report in accordance with the journal’s patient consent policy.
Supplementary Files
Supplementary file 1. Coronary Angiography - Pathologic Left Anterior Oblique (LAO) Cranial View Progression (CSFP observed)
(gif)
Supplementary file 2. Coronary Angiography - Pathologic LAO Caudal View Progression (CSFP observed)
(gif)
Supplementary file 3: Coronary Angiography - Normal LAO Cranial View
(gif)
Supplementary file 4: Coronary Angiography - Normal LAO Caudal View
(gif)
Acknowledgements
The authors would like to express their gratitude to Mashhad University of Medical Sciences.
References
- Tambe AA, Demany MA, Zimmerman HA, Mascarenhas E. Angina pectoris and slow flow velocity of dye in coronary arteries--a new angiographic finding. Am Heart J 1972; 84(1):66-71. doi: 10.1016/0002-8703(72)90307-9 [Crossref] [ Google Scholar]
- Wang X, Nie SP. The coronary slow flow phenomenon: characteristics, mechanisms and implications. Cardiovasc Diagn Ther 2011; 1(1):37-43. doi: 10.3978/j.issn.2223-3652.2011.10.01 [Crossref] [ Google Scholar]
- Mosseri M, Yarom R, Gotsman MS, Hasin Y. Histologic evidence for small-vessel coronary artery disease in patients with angina pectoris and patent large coronary arteries. Circulation 1986; 74(5):964-72. doi: 10.1161/01.cir.74.5.964 [Crossref] [ Google Scholar]
- Chalikias G, Tziakas D. Slow coronary flow: pathophysiology, clinical implications, and therapeutic management. Angiology 2021; 72(9):808-18. doi: 10.1177/00033197211004390 [Crossref] [ Google Scholar]
- Mikaeilvand A, Hajizadeh R, Bateni A, Yahyapour Z. Long-term prognosis in patients with coronary slow flow. J Tehran Heart Cent 2022; 17(4):202-6. doi: 10.18502/jthc.v17i4.11608 [Crossref] [ Google Scholar]
- Beltrame JF, Limaye SB, Wuttke RD, Horowitz JD. Coronary hemodynamic and metabolic studies of the coronary slow flow phenomenon. Am Heart J 2003; 146(1):84-90. doi: 10.1016/s0002-8703(03)00124-8 [Crossref] [ Google Scholar]
- Hawkins BM, Stavrakis S, Rousan TA, Abu-Fadel M, Schechter E. Coronary slow flow--prevalence and clinical correlations. Circ J 2012; 76(4):936-42. doi: 10.1253/circj.cj-11-0959 [Crossref] [ Google Scholar]
- Sanghvi S, Mathur R, Baroopal A, Kumar A. Clinical, demographic, risk factor and angiographic profile of coronary slow flow phenomenon: a single centre experience. Indian Heart J 2018; 70(Suppl 3):S290-4. doi: 10.1016/j.ihj.2018.06.001 [Crossref] [ Google Scholar]
- Aciksari G, Cetinkal G, Kocak M, Atici A, Celik FB, Caliskan M. The relationship between triglyceride/high-density lipoprotein cholesterol ratio and coronary slow-flow phenomenon. Int J Cardiovasc Imaging 2022; 38(1):5-13. doi: 10.1007/s10554-021-02387-w [Crossref] [ Google Scholar]
- Zavala-Alarcon E, Cecena F, Little R, Bant A, Van Poppel S, Patel R. The no-flow phenomenon during diagnostic coronary angiography. Cardiovasc Revasc Med 2005; 6(3):126-32. doi: 10.1016/j.carrev.2005.07.007 [Crossref] [ Google Scholar]
- Huang Q, Zhang F, Chen S, Dong Z, Liu W, Zhou X. Clinical characteristics in patients with coronary slow flow phenomenon: a retrospective study. Medicine (Baltimore) 2021; 100(6):e24643. doi: 10.1097/md.0000000000024643 [Crossref] [ Google Scholar]
- Nurkalem Z, Tangurek B, Zencirci E, Alper AT, Aksu H, Erer B. Endothelial nitric oxide synthase gene (T-786C) polymorphism in patients with slow coronary flow. Coron Artery Dis 2008; 19(2):85-8. doi: 10.1097/MCA.0b013e3282f52940 [Crossref] [ Google Scholar]
- Ozdogru I, Zencir C, Dogan A, Orscelik O, Inanc MT, Celik A. Acute effects of intracoronary nitroglycerin and diltiazem in coronary slow flow phenomenon. J Investig Med 2013; 61(1):45-9. doi: 10.2310/JIM.0b013e318279b7f6 [Crossref] [ Google Scholar]
- Xia T, Guan W, Fu J, Zou X, Han Y, Chen C. Tirofiban induces vasorelaxation of the coronary artery via an endothelium-dependent NO-cGMP signaling by activating the PI3K/Akt/eNOS pathway. Biochem Biophys Res Commun 2016; 474(3):599-605. doi: 10.1016/j.bbrc.2016.03.110 [Crossref] [ Google Scholar]
- Simsek H, Yaman M, Babat N, Akdag S, Akyol A, Demirel KC. Decreased risk of ventricular arrhythmias with treatment of nebivolol in patients with coronary slow flow. Kardiol Pol 2016; 74(10):1174-9. doi: 10.5603/KP.a2016.0060 [Crossref] [ Google Scholar]
- Beltrame JF. Defining the coronary slow flow phenomenon. Circ J 2012; 76(4):818-20. doi: 10.1253/circj.cj-12-0205 [Crossref] [ Google Scholar]
- Cin VG, Pekdemir H, Camsar A, Ciçek D, Akkus MN, Parmaksýz T. Diffuse intimal thickening of coronary arteries in slow coronary flow. Jpn Heart J 2003; 44(6):907-19. doi: 10.1536/jhj.44.907 [Crossref] [ Google Scholar]
- Beltrame JF, Limaye SB, Horowitz JD. The coronary slow flow phenomenon--a new coronary microvascular disorder. Cardiology 2002; 97(4):197-202. doi: 10.1159/000063121 [Crossref] [ Google Scholar]
- Gibson CM, Cannon CP, Daley WL, Dodge JT Jr, Alexander B Jr, Marble SJ. TIMI frame count: a quantitative method of assessing coronary artery flow. Circulation 1996; 93(5):879-88. doi: 10.1161/01.cir.93.5.879 [Crossref] [ Google Scholar]
- Sadamatsu K, Koga Y, Tashiro H. Long-term follow-up of patients with coronary slow flow phenomenon. Am J Cardiovasc Drugs 2018; 18(1):73-4. doi: 10.1007/s40256-017-0241-4 [Crossref] [ Google Scholar]
- Sadr-Ameli MA, Saedi S, Saedi T, Madani M, Esmaeili M, Ghardoost B. Coronary slow flow: benign or ominous?. Anatol J Cardiol 2015; 15(7):531-5. doi: 10.5152/akd.2014.5578 [Crossref] [ Google Scholar]
- Alvarez C, Siu H. Coronary slow-flow phenomenon as an underrecognized and treatable source of chest pain: case series and literature review. J Investig Med High Impact Case Rep 2018; 6:2324709618789194. doi: 10.1177/2324709618789194 [Crossref] [ Google Scholar]
- Weferling M, Vietheer J, Keller T, Fischer-Rasokat U, Hamm CW, Liebetrau C. Association between primary coronary slow-flow phenomenon and epicardial fat tissue. J Invasive Cardiol 2021; 33(1):E59-64. doi: 10.25270/jic/20.00294 [Crossref] [ Google Scholar]
- Afsin A, Kaya H, Suner A, Uzel KE, Bursa N, Hosoglu Y. Plasma atherogenic indices are independent predictors of slow coronary flow. BMC Cardiovasc Disord 2021; 21(1):608. doi: 10.1186/s12872-021-02432-5 [Crossref] [ Google Scholar]
- Seyyed Mohammadzad MH, Khademvatani K, Gardeshkhah S, Sedokani A. Echocardiographic and laboratory findings in coronary slow flow phenomenon: cross-sectional study and review. BMC Cardiovasc Disord 2021; 21(1):230. doi: 10.1186/s12872-021-02044-z [Crossref] [ Google Scholar]
- Pekdemir H, Cin VG, Ciçek D, Camsari A, Akkus N, Döven O. Slow coronary flow may be a sign of diffuse atherosclerosis Contribution of FFR and IVUS. Acta Cardiol 2004; 59(2):127-33. doi: 10.2143/ac.59.2.2005166 [Crossref] [ Google Scholar]
- Binak E, Gunduz H, Sahin M, Kurtoglu N, Dindar I. The relation between impaired glucose tolerance and slow coronary flow. Int J Cardiol 2006; 111(1):142-6. doi: 10.1016/j.ijcard.2005.09.007 [Crossref] [ Google Scholar]
- Sezgin AT, Barutcu I, Sezgin N, Gullu H, Esen AM, Acikgoz N. Contribution of plasma lipid disturbances to vascular endothelial function in patients with slow coronary flow. Angiology 2006; 57(6):694-701. doi: 10.1177/0003319706295472 [Crossref] [ Google Scholar]
- Mukhopadhyay S, Kumar M, Yusuf J, Gupta VK, Tyagi S. Risk factors and angiographic profile of coronary slow flow (CSF) phenomenon in North Indian population: an observational study. Indian Heart J 2018; 70(3):405-9. doi: 10.1016/j.ihj.2017.09.001 [Crossref] [ Google Scholar]