J Cardiovasc Thorac Res. 17(1):1-11.
doi: 10.34172/jcvtr.025.33280
Review Article
Efficacy of flaxseed in reducing blood pressure among patients with cardiovascular risk factors: A systematic review and meta-analysis of parallel randomized controlled trials
Refli Hasan Conceptualization, Methodology, Project administration, Supervision, Validation, Visualization, Writing – original draft, Writing – review & editing, 1, * 
Raed Obaid Saleh Conceptualization, Methodology, Project administration, Supervision, Validation, Visualization, Writing – original draft, Writing – review & editing, 2, * 
Rana H. Raheema Data curation, Investigation, Methodology, Resources, Writing – original draft, 3
Hanen Mahmod Hulail Data curation, Investigation, Methodology, Resources, Writing – original draft, 4
Irfan Ahmad Formal analysis, Funding acquisition, Methodology, Software, Writing – original draft, Writing – review & editing, 5, 6
Deepak Nathiya Formal analysis, Methodology, Software, Writing – original draft, Writing – review & editing, 7
Parjinder Kaur Formal analysis, Methodology, Software, Writing – original draft, Writing – review & editing, 8
Author information:
1Department of Internal Medicine, Faculty of Medicine, Universitas Sumatera Utara, Medan, Indonesia
2Medical Laboratory Techniques Department, College of Health and Medical Technology, University of Al Maarif, Anbar, Iraq
3Department of Medical Microbiology, College of Medicine, Wasit University, Kut, Iraq
4Department of Medical Laboratories Technology, AL-Nisour University College, Baghdad, Iraq
5Central Labs, King Khalid University, AlQura’a, Abha, Saudi Arabia
6Department of Clinical Laboratory Sciences, College of Applied Medical Sciences, King Khalid University, Abha, Saudi Arabia
7Department of Pharmacy Practice, NIMS Institute of Pharmacy, NIMS University Rajasthan, Jaipur, India
8Chandigarh Pharmacy College, Chandigarh Group of Colleges-Jhanjeri, Mohali 140307, Punjab, India
Abstract
The prevalence rate of hypertension is on the rise at an alarming rate. Studies conducted on the influence of flaxseed on blood pressure (BP) have come up with conflicting conclusions. The current investigation’s major purpose is to conduct a literature review and a meta-analysis focusing on the effect of flaxseed supplementation on BP in people with cardiovascular disease (CVD) risk factors. PubMed, Scopus, Web of Science, and Cochrane Central Library databases were searched from the inception date to April 2024 to find the randomized controlled trials (RCTs). A random-effects model combined the weighted mean difference (WMD). Standard methodologies were applied to evaluate publication bias, heterogeneity, and sensitivity analysis. Eighteen RCTs were included in the present systematic review and meta-analysis. Pooled analysis suggested that flaxseed supplementation can reduce systolic BP (SBP) (WMD: -4.75 mmHg, 95% CI: -7.05 to -2.44, P≤0.001; I2=93.6%) and diastolic BP (DBP) (WMD: -3.09 mmHg, 95% CI: -4.37 to -1.81, P≤0.001; I2=91.2%). In conclusion, the current meta-analysis has demonstrated that flaxseed supplementation can markedly lower BP in individuals exhibiting CVD risk factors. Given the significant heterogeneity, it is crucial to interpret the current results with careful consideration. In addition, further high-quality RCTs are required to better assess the causal relationships.
Keywords: Flaxseed, Blood pressure, Cardiovascular disease, Systematic review, Meta-analysis
Copyright and License Information
© 2025 The Author(s).
This is an open access article distributed under the terms of the Creative Commons Attribution License (
http://creativecommons.org/licenses/by/4.0/), which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited.
Funding Statement
This study is supported via funding from King Khalid University, Abha, Saudi Arabia under Grant no. R.G.P.2/517/45.
Introduction
Cardiovascular disease (CVD) is the foremost cause of mortality across the globe, making it a critical public health concern. Significant cardiovascular risk determinants encompass factors such as obesity, age, sex, dyslipidemia, metabolic syndrome (MetS), and type 2 diabetes mellitus (T2DM).1,2 Another significant risk factor for cardiovascular and renal diseases is hypertension (HTN). It is estimated that 1.3 billion adults worldwide have HTN, and it is mostly prevalent in low- and middle-income countries. HTN is present in about 25% of the adult population and only one-third of these patients manage to control their blood pressure (BP).3 Therefore, controlling BP is crucial for any healthcare system as HTN incurs significant costs for the government and a burden on the community.3,4 According to experts, a combination of lifestyle changes, such as increased consumption of fruits, low-fat dairy, vegetables, sodium reduction, and exercise together with medication is critical in the management of BP.5-7 Due to the various adverse effects of pharmaceutical therapy, nutrition therapy has gained increasing attention in recent years.8-10 In this sense, herbal treatments become important due to their efficacy in treating high BP and their low cost.11-14 It’s important to note that herbal compounds should be used as a complementary solution alongside aforesaid approaches to control BP.15-17
Flaxseed also known as linseed (Linum usitatissimum) is a functional food rich in alpha-linolenic acid (ALA) and effective phytochemicals including lignan, phenolic acids, phytoestrogens, and flavonoids.18,19 It possesses several properties such as antioxidant,20 anti-atherosclerotic,18,21-23 anti-obesity,24 anti-diabetic,25 anti-microbial,26 anti-cancer 27, anti-arthritic28 and anti-inflammatory.21 Given the aforementioned properties and the high content of polyunsaturated fatty acids (PUFA) in flaxseed, it is anticipated that flaxseed may also be effective in improving BP. A multitude of trials has been conducted to assess the efficacy of flaxseed and its derivatives in regulating BP among human subjects.29-46 However, the results of the existing clinical trials have been inconsistent, and the differences might be due to various aspects of the study design, such as study power, the recruitment of patients, sample size, study duration, and the dose of flaxseed or its derivatives used. Previous meta-analyses47-49 in this field have combined studies involving both healthy and non-healthy individuals. Baseline BP levels can differ significantly between healthy individuals and those suffering from metabolic disorders, thereby influencing the results of these investigations. Additionally, no research has specifically focused on the effects of flaxseeds on individuals with risk factors for heart disease. In present analysis, only studies employing a parallel design were considered, as variations in study design may significantly affect the outcomes.
This systematic review and meta-analysis aim to examine the scientific evidence regarding the effects of flaxseed supplementation on BP in patients with CVD risk factors.
Methods
We followed the Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA) guidelines to conduct and report this paper.50
Literature Search
The following global scientific databases were explored for pertinent articles published until April 2024: Cochrane Central Library, Web of Science, Scopus, and PubMed. The subsequent keywords were utilized in the search: (flax OR flaxseed OR linseed OR lignan OR Linum usitatissimum) AND (BP OR blood pressure OR SBP OR systolic blood pressure OR DBP OR diastolic blood pressure OR hypertension). In the search strategy, we included the aforementioned MeSH terms and keywords without language limitations. In addition, we searched through the references of the articles that were included and recent reviews to identify papers that fulfilled the eligibility requirements. The complete search strategies are presented in Supplementary file, Table S1.
Study selection
Two researchers (R.HR. and I.A) conducted an independent examination of titles, abstracts, and subsequently, full texts to identify potentially qualifying articles. Any discrepancies were resolved through consensus with the third author (P.K). The following criteria were used to include eligible studies in this meta-analysis: (1) the studies should be randomized controlled trials (RCTs) with a parallel design; (2) they should investigate the effect of flaxseed on BP among individuals exhibiting risk factors for CVD such as dyslipidemia, T2DM, MetS, HTN, pre-diabetes, nonalcoholic fatty liver (NAFLD), or obesity; (3) they should provide baseline and end-trial BP measurements for both flaxseed and control groups; and (4) they must involve a flaxseed supplementation duration of no less than one week., Trials that did not provide adequate data regarding BP measurements for both intervention and control groups as well as non-clinical studies, and uncontrolled RCTs were excluded from present meta-analysis. Furthermore, studies examining the effects of flaxseed in conjunction with other interventions such as herbs or substances, as well as those involving children, adolescents, pregnant women, and lactating women, were also excluded.
Data extraction
The data was meticulously extracted through the utilization of a standardized form that was specifically designed to ensure consistency and accuracy in the collection process. Two investigators (D.N and H.M.H) conducted an independent assessment of each manuscript that satisfied the established eligibility criteria and gathered the following pertinent information: the surname of the primary author, the year of publication, the geographical setting, mean age, body mass index (BMI), and gender of participants, duration of follow-up, overall sample size, dose, type of flaxseed and control group, the overall health condition of participants, as well as the mean and standard deviation (SD) of SBP and DBP at both the baseline and concluding phases of the research. Any discrepancies were resolved through the agreement reached by the third author (P.K).
Quality assessment
The Cochrane Risk of Bias tool51 was employed to assess the methodological quality of the included RCTs. This instrument comprised seven distinct domains: random sequence generation, allocation concealment, blinding of participants and personnel, blinding of outcome assessment, incomplete outcome data, selective reporting, and other sources of bias. Each domain was categorized as exhibiting a low, high, or unclear risk of bias. Two independent reviewers (D.N and H.M.H) conducted a thorough evaluation of the assessment’s methodological quality, ensuring a rigorous and unbiased analysis, and any discrepancies identified in the Cochrane Risk of Bias ratings were addressed through discussion.
Evaluation of evidence strength
The assurance of evidence was appraised employing the Grading of Recommendations Assessment, Development, and Evaluation (GRADE) framework. This assessment focused on several domains: risk of bias, inconsistency, indirectness, imprecision, and publication bias.52 The quality of the evidence was rated as high, moderate, low and very low.
Statistical analysis
In the initial analysis, we assessed the intergroup variations in BP alterations between the flaxseed and control groups, subsequently aggregating these findings. The effect size was examined through the application of the weighted mean difference (WMD) alongside a 95% confidence interval (CI). The data were subjected to analysis utilizing a random-effects model, which facilitated the possibility that the true effect may differ across various studies. The statistical heterogeneity was evaluated using the I2 index. We considered a value greater than 50% as denoting substantial heterogeneity. We performed a subgroup analysis to evaluate the influence of the intervention duration and the participants’ health status on the resultant outcomes. A non-linear dose-response analysis was conducted to examine the relationship between overall effect size and flaxseed dosage (g/day). The sensitivity of the findings to individual studies was scrutinized by systematically omitting one publication at a time from the analysis. In order to assess the potential existence of publication bias, the Egger’s test was employed. The computer software “STATA, version 11.2 (Stata Corp., College Station, TX, USA)” was employed for the execution of the meta-analyses of the data, with all statistical tests being two-sided and a significance level established at 0.05, unless indicated otherwise.
Results
Summary of included studies
Out of the 1790 articles that were initially identified, only 43 full-text articles underwent a detailed evaluation. Nonetheless, 25 of these investigations were excluded for a variety of reasons (as illustrated in Figure 1). Consequently, only 18 articles,29-46 encompassing a total of 1298 subjects, fulfilled the inclusion criteria and were selected for subsequent qualitative and quantitative analysis.
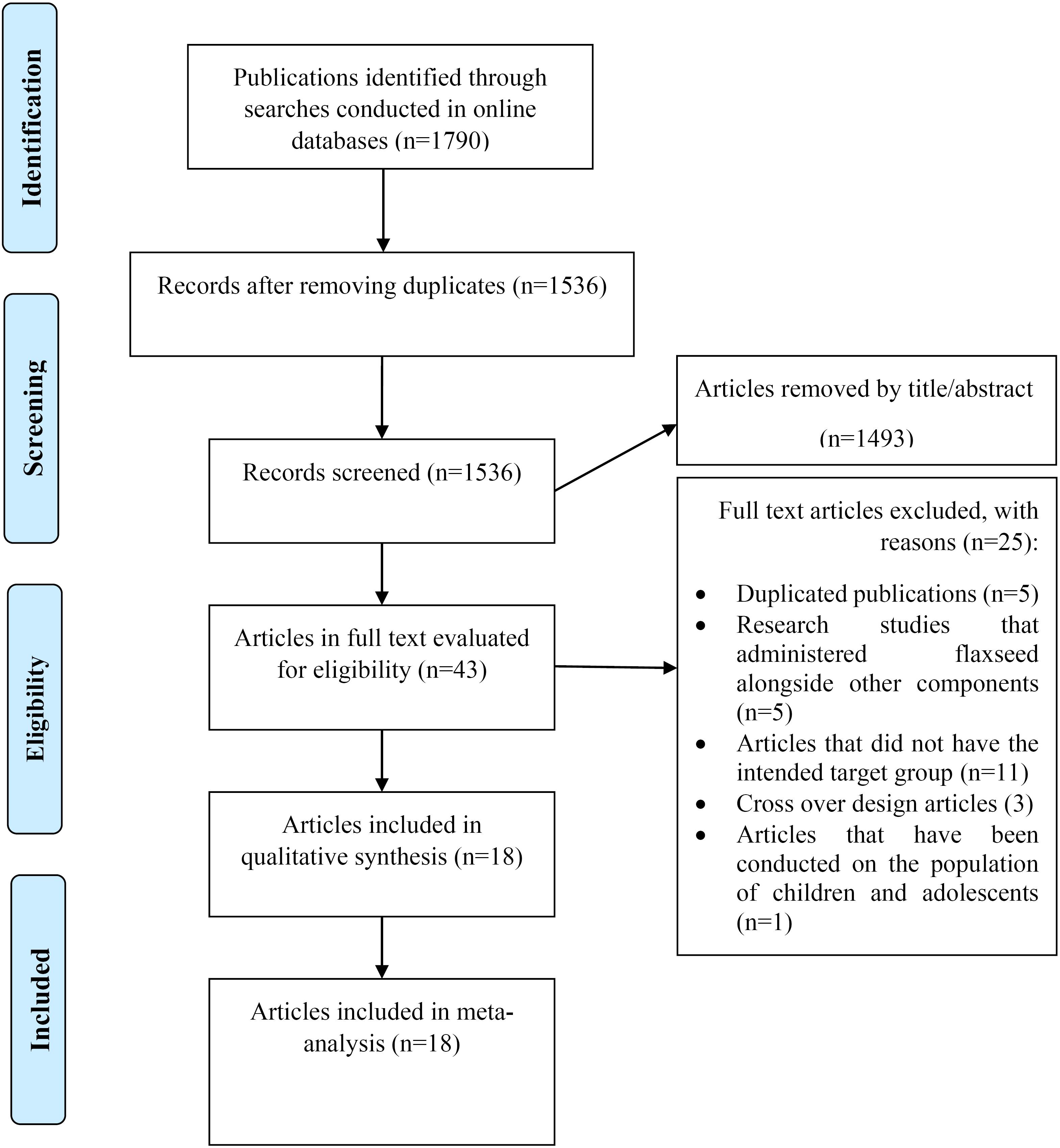
Figure 1.
Flow diagram of the literature and screening process
.
Flow diagram of the literature and screening process
Characteristics of the studies
Table 1 presents a comprehensive overview of the essential characteristics of the included papers. These articles were published between 2010 and 2022. A total of nine investigations were executed within the geographical confines of Iran, while three were undertaken in China. The remaining research engagements were carried out in India, Brazil, the United States of America, the Netherlands, and Cuba, respectively. The average age of the participants spanned from 22 to 66 years, and the baseline BMI exhibited variability from 23 to 32 kg/m2. One of the studies had male-only subjects while the remaining were with both genders. The time duration of included RCTs varied from 6 weeks to three months. Included studies were conducted in various populations, including subjects with coronary artery disease, T2DM, HTN, pre-diabetes, dyslipidemia, obesity, MetS, and NAFLD.
Table 1.
Study characteristics of included studies
First author
(publication year, country)
|
Total participants (gender)
|
Mean age
(year)
|
Mean BMI
(kg/m2)
|
Duration
(week)
|
Health condition
|
Intervention
|
Control
|
Bhardwaj 30
(2022, India) a |
76 (Male/Female) |
57 |
25 |
24 |
Coronary artery disease |
Blended flaxseed oil (30 g/d) |
Sunflower oil |
Bhardwaj 30
(2022, India) b |
76 (Male/Female) |
57.5 |
23 |
24 |
Hypertension |
Blended flaxseed oil (30 g/d) |
Sunflower oil |
Toulabi 42
(2022, Iran) |
76 (Male/Female) |
52 |
29 |
12 |
Hypertension |
Flaxseed (30 g/d) |
Wheat flour |
Yari 45
(2021, Iran) a |
47 (Male/Female) |
45 |
31 |
12 |
Metabolic syndrome |
whole flaxseed (30 g/d) + lifestyle intervention |
lifestyle intervention |
Yari 45
(2021, Iran) b |
44 (Male/Female) |
45 |
31 |
12 |
Metabolic syndrome |
whole flaxseed (30 g/d) + hesperidin (1 g/d) + lifestyle intervention |
lifestyle intervention + hesperidin (1 g/d) |
Rezaei 39
(2020, Iran) |
68 (Male/Female) |
43 |
30 |
12 |
NAFLD |
Flaxseed oil (20 g/d) |
Sunflower oil |
Kuang 37
(2020, China) |
51 (Male/Female) |
22 |
26 |
8 |
Overweight and obese |
Flaxseed meal (100g/d) |
Control biscuits |
Yang 44
(2019, China) |
74 (Male/Female) |
57 |
26 |
12 |
Hypertension |
Flaxseed oil (2.5 g/d) |
Corn oil |
Pieters 38
(2019, Netherlands) |
59 (Male/Female) |
60 |
30 |
12 |
Overweight and obese |
Refined cold-pressed flaxseed oil (1 g/d) |
Sunflower oil |
Saleh-Ghadimi 41
(2019, Iran) |
40 (Male/Female) |
55 |
30 |
10 |
Coronary artery disease |
Flaxseed oil (5 g/d) |
Milk |
Hasaniani 34
(2019, Iran) |
57 (Male/Female) |
53 |
29 |
8 |
T2DM |
Flaxseed (30 g/d) |
Plain yogurt |
Haghighatsiar 33
(2019, Iran) |
80 (Male/Female) |
43 |
28 |
8 |
Dyslipidemic and
hypertensive patients |
Flaxseed sachet (36g/d) |
Placebo sachet |
Akrami 29
(2017, Iran) |
52 (Male/Female) |
48 |
NR |
7 |
Metabolic syndrome |
Flaxseed oil (25 ml/d) |
Sunflower oil |
Yari 46
(2016, Iran) |
44 (Male/Female) |
45 |
30 |
12 |
Metabolic syndrome |
Brown milled flaxseed (30g/d) |
lifestyle advice |
Javidi 35
(2016, Iran) |
62 (Male/Female) |
51 |
27 |
12 |
Prediabetic |
Flaxseed powder (40 g/d) |
Control |
Cassani 31
(2015, Brazil) |
27 (Male) |
36 |
32 |
6 |
Cardiovascular risk factors |
Flaxseed powder (60 g/d) |
Raw rice powder |
Katare 36
(2013, India) |
50 (Male/Female) |
52 |
28 |
12 |
Dyslipidemia |
Roasted flaxseed powder (30 g/d) |
Control |
Rodriguez-Leyva 40
(2013, Cuba) |
86 (Male/Female) |
66 |
NR |
24 |
Hypertension |
Milled flaxseed (30g/d) |
Wheat flour |
Dewell 32
(2011, USA) |
40 (Male/Female) |
49 |
30 |
8 |
Metabolic syndrome |
Flaxseed oil (6.6 g/d) |
Soybean oil |
Wu 43
(2010, China) |
189 (Male/Female) |
48 |
25 |
12 |
Metabolic syndrome |
Flaxseed (30g/d) + lifestyle counseling |
Lifestyle counseling |
BMI, body mass index; T2DM, type 2 diabetes mellitus; NAFLD, nonalcoholic fatty liver; NR, not reported
Risk of bias, and grade assessment
Most of the included publications were of high methodological quality, according to the Cochrane Risk of Bias checklist. Comprehensive information regarding the quality assessment is reported in Table 2. According to the GRADE approach both outcomes were rated at moderate levels of evidence. The level of evidence was downgraded due to serious imprecision limitations. More details of grade assessment are showed in Table 3.
Table 2.
Literature quality assessment based on Cochrane guidelines
First author
(publication year)
|
Random Sequence Generation
|
Allocation concealment
|
Blinding of participants, personnel
|
Blinding of outcome assessment
|
Incomplete outcome data
|
Selective outcome reporting
|
Other sources of bias
|
| Bhardwaj 30 (2022) |
L |
L |
L |
H |
L |
L |
H |
| Toulabi 42 (2022) |
L |
L |
L |
L |
L |
L |
L |
| Yari 45 (2021) |
L |
U |
L |
L |
U |
U |
L |
| Rezaei 39 (2020) |
L |
L |
L |
H |
L |
L |
L |
| Kuang 37 (2020) |
L |
L |
L |
H |
L |
L |
L |
| Yang 44 (2019) |
L |
L |
L |
L |
L |
L |
L |
| Pieters 38 (2019) |
L |
L |
L |
H |
L |
L |
L |
| Saleh-Ghadimi 41 (2019) |
L |
L |
L |
L |
L |
L |
L |
| Hasaniani 34 (2019) |
L |
H |
L |
H |
L |
L |
L |
| Haghighatsiar 33 (2019) |
L |
L |
L |
L |
L |
L |
L |
| Akrami 29(2017) |
L |
L |
L |
H |
U |
L |
U |
| Yari 46 (2016) |
L |
U |
L |
L |
U |
U |
L |
| Javidi 35 (2016) |
L |
L |
L |
H |
U |
L |
L |
| Cassani 31 (2015) |
L |
L |
L |
H |
H |
U |
L |
| Katare 36 (2013) |
U |
U |
L |
H |
U |
U |
U |
| Rodriguez-Leyva 40 (2013) |
L |
L |
L |
H |
L |
L |
U |
| Dewell 32 (2011) |
L |
U |
L |
H |
U |
U |
L |
| Wu 43 (2010) |
L |
L |
L |
U |
L |
U |
U |
U, unclear risk of bias; L, low risk of bias; H, high risk of bias
Table 3.
Quality of the evidence evaluated by GRADE
|
Outcome
|
Certainty assessment
|
Certainty
|
|
Risk of bias
|
Inconsistency
|
Indirectness
|
Imprecision
|
Publication bias
|
| SBP |
No serious limitation |
No serious limitation |
No serious limitation |
Serious limitation |
No serious limitation |
⨁⨁◯⨁ Moderate |
| DBP |
No serious limitation |
No serious limitation |
No serious limitation |
Serious limitation |
No serious limitation |
⨁⨁◯⨁ Moderate |
SBP, systolic blood pressure; DBP, diastolic blood pressure
Effect of flaxseed supplementation on systolic blood pressure
A comprehensive analysis of 18 trials which included 20 arms, suggested significant benefits to flaxseed supplementation regarding systolic BP (SBP) levels (WMD: -4.75 mmHg, 95% CI: -7.05 to -2.44, P ≤ 0.001). However, the analysis indicated significant heterogeneity between these 18 trials (I2 = 93.6%, P < 0.001) (Figure 2). When studies were evaluated based on the study duration or the health status of the participants, a significant effect was recorded on SBP in all subgroups except in subjects who had dyslipidemia (WMD: -1.49 mmHg, 95% CI: -3.32 to 0.34, P = 0.1). Furthermore, heterogeneity between studies in subsets of participants with MetS and dyslipidemia decreased significantly (I2 = 37.2%, P = 0.15 and I2 = 38.9%, P = 0.20; respectively) (Table 4).
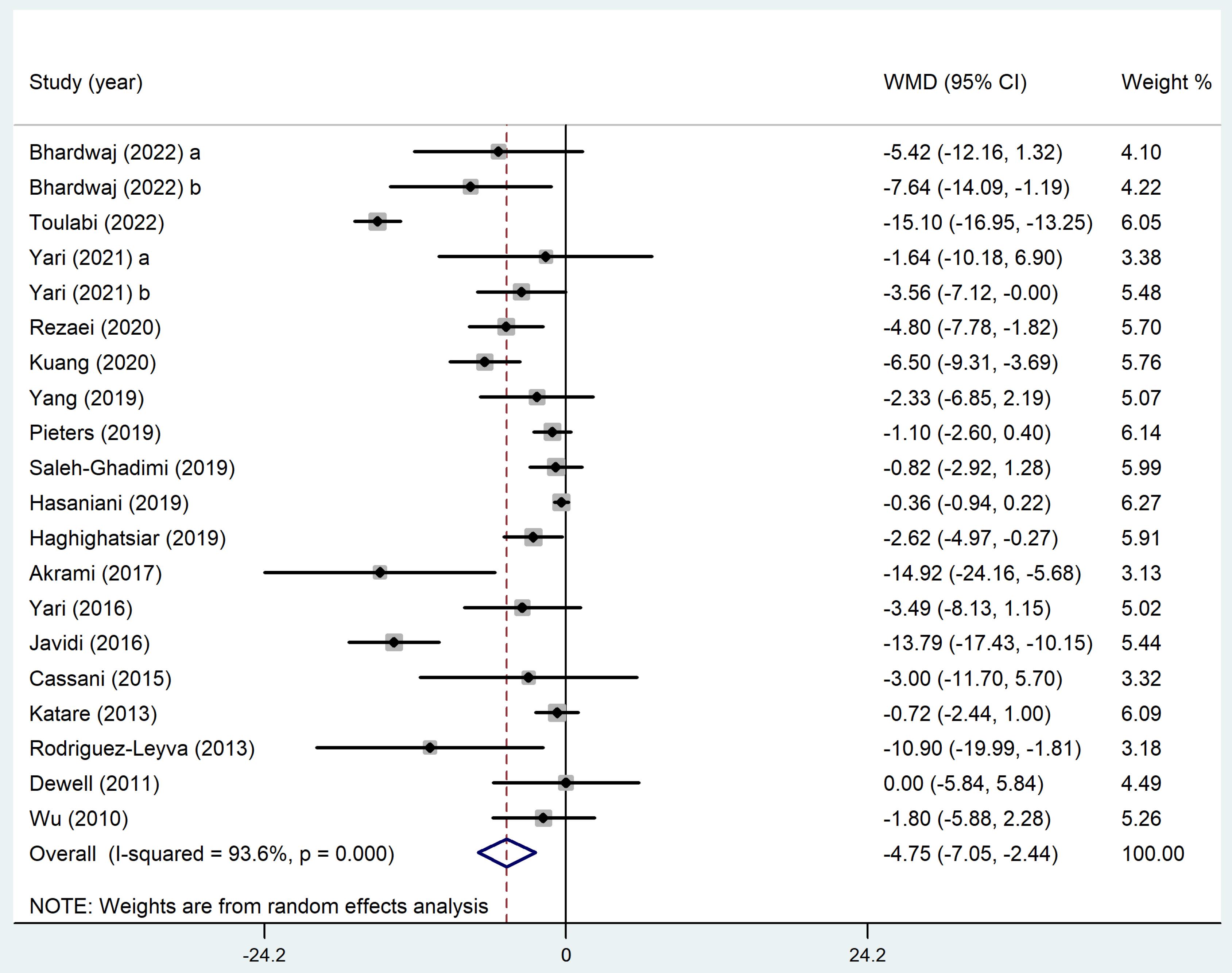
Figure 2.
Forest plot illustrating the impact of flaxseed supplementation on systolic blood pressure in participants with cardiovascular disease risk factors
.
Forest plot illustrating the impact of flaxseed supplementation on systolic blood pressure in participants with cardiovascular disease risk factors
Table 4.
Result of subgroup analysis of included studies in meta-analysis.
|
Sub-grouped by
|
No. of arms
|
Effect size1
|
95% CI
|
P for effect size
|
I2 (%)
|
P for heterogeneity
|
|
SBP
|
| Health status |
| Dyslipidemia |
2 |
-1.49 |
(-3.32 to 0.34) |
0.1 |
38.9% |
0.20 |
| Hypertension |
4 |
-9.06 |
(-16.41 to -1.70) |
0.01 |
89.7% |
˂0.001 |
| Metabolic syndrome |
6 |
-3.29 |
(-6.03 to -0.55) |
0.01 |
37.2% |
0.15 |
| Other |
8 |
-4.20 |
(-6.76 to -1.63) |
0.001 |
90.7% |
˂0.001 |
| Intervention duration |
| > 10 weeks |
13 |
-5.51 |
(-9.06 to -1.96) |
0.002 |
93.8% |
˂0.001 |
| ≤ 10 weeks |
7 |
-2.80 |
(-5.11 to -0.49) |
0.01 |
79.8% |
˂0.001 |
|
DBP
|
| Health status |
| Dyslipidemia |
2 |
-0.84 |
(-1.61 to -0.07) |
0.03 |
0.0% |
0.76 |
| Hypertension |
4 |
-7.05 |
(-11.28 to -2.83) |
0.001 |
83.7% |
˂0.001 |
| Metabolic syndrome |
6 |
-1.24 |
(-2.42 to -0.05) |
0.04 |
0.0% |
0.82 |
| Other |
8 |
-3.27 |
(-5.34 to -1.21) |
0.002 |
95.1% |
˂0.001 |
| Intervention duration |
| > 10 weeks |
13 |
-3.81 |
(-5.51 to -2.11) |
˂0.001 |
89.7% |
˂0.001 |
| ≤ 10 weeks |
7 |
-1.65 |
(-4.01 to 0.71) |
0.17 |
92.2% |
˂0.001 |
1Calculated by Random-effects model
Effect of flaxseed supplementation on diastolic blood pressure
A total of 18 studies (20 arms) reported diastolic BP (DBP) outcomes. The overall WMD analyzed through a random-effects model indicated a statistically significant improvement in DBP among subjects receiving flaxseed compared to the control group (WMD: -3.09 mmHg, 95% CI: -4.37 to -1.81, P ≤ 0.001). Nevertheless, it is important to note that there existed significant heterogeneity among the RCTs (I2 = 91.2%, P < 0.001)(Figure 3). In order to find out the source of this heterogeneity, sub-group analysis was done. The findings indicated that flaxseed was effective in lowering DBP in all subgroups, except for interventions lasting less than 10 weeks (WMD: -1.65 mmHg, 95% CI: -4.01 to 0.71, P = 0.17). In addition, the heterogeneity among studies in the subgroup of subjects with MetS and dyslipidemia dropped immensely (I2 = 0.0%, P = 0.82 and I2 = 0.0%, P = 0.76, respectively)(Table 4).
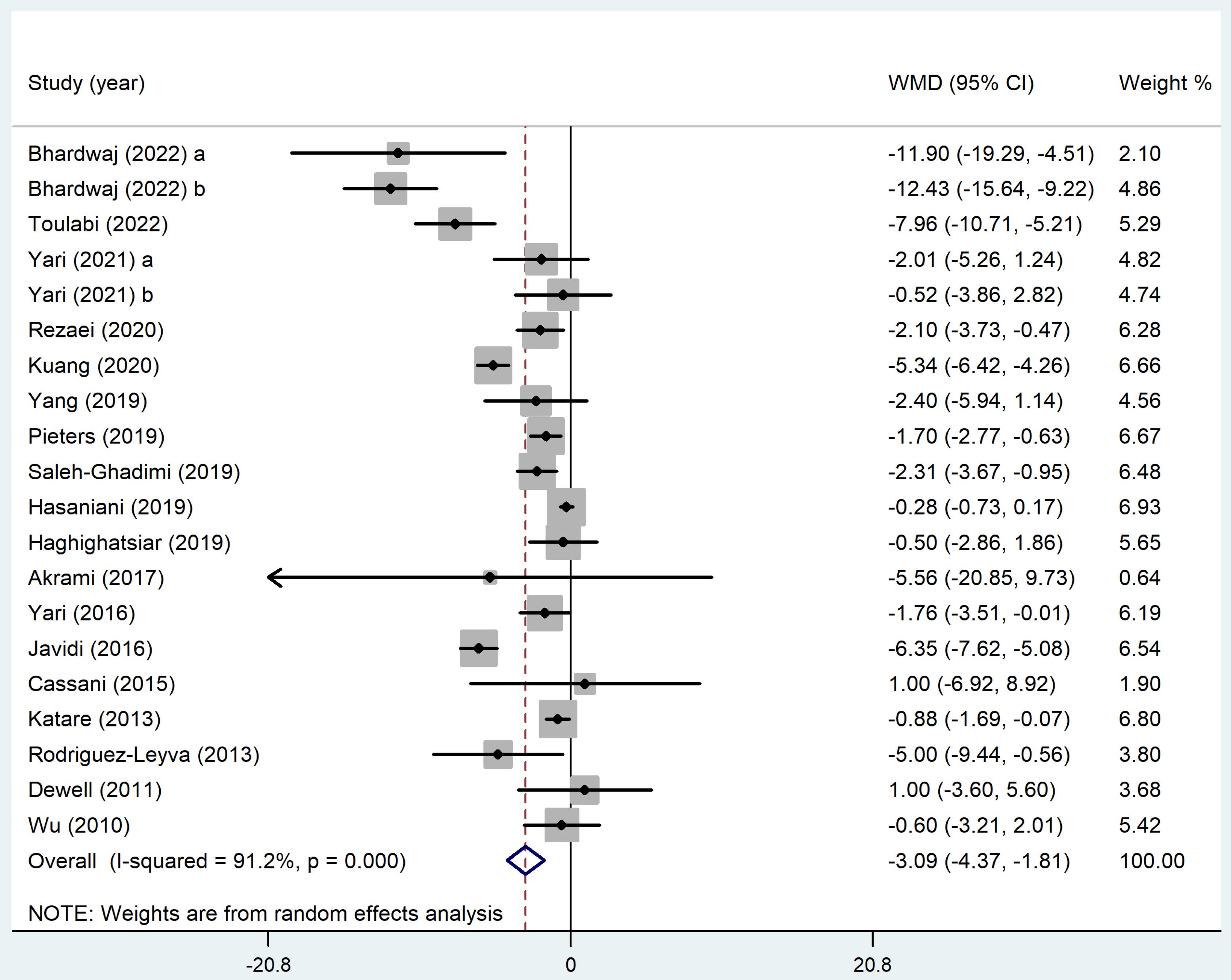
Figure 3.
Forest plot illustrating the impact of flaxseed supplementation diastolic blood pressure in participants with cardiovascular disease risk factors
.
Forest plot illustrating the impact of flaxseed supplementation diastolic blood pressure in participants with cardiovascular disease risk factors
Dose-response analyses
Dose-response analysis indicated that flaxseed supplementation did not significantly affect SBP (P = 0.15) and DBP (P = 0.64) levels based on the dosage. It can be concluded from the dose-response analysis that the optimum level of flaxseed that leads to the greatest observed changes in SBP and DBP was 30 grams daily (Figures 4 and 5).
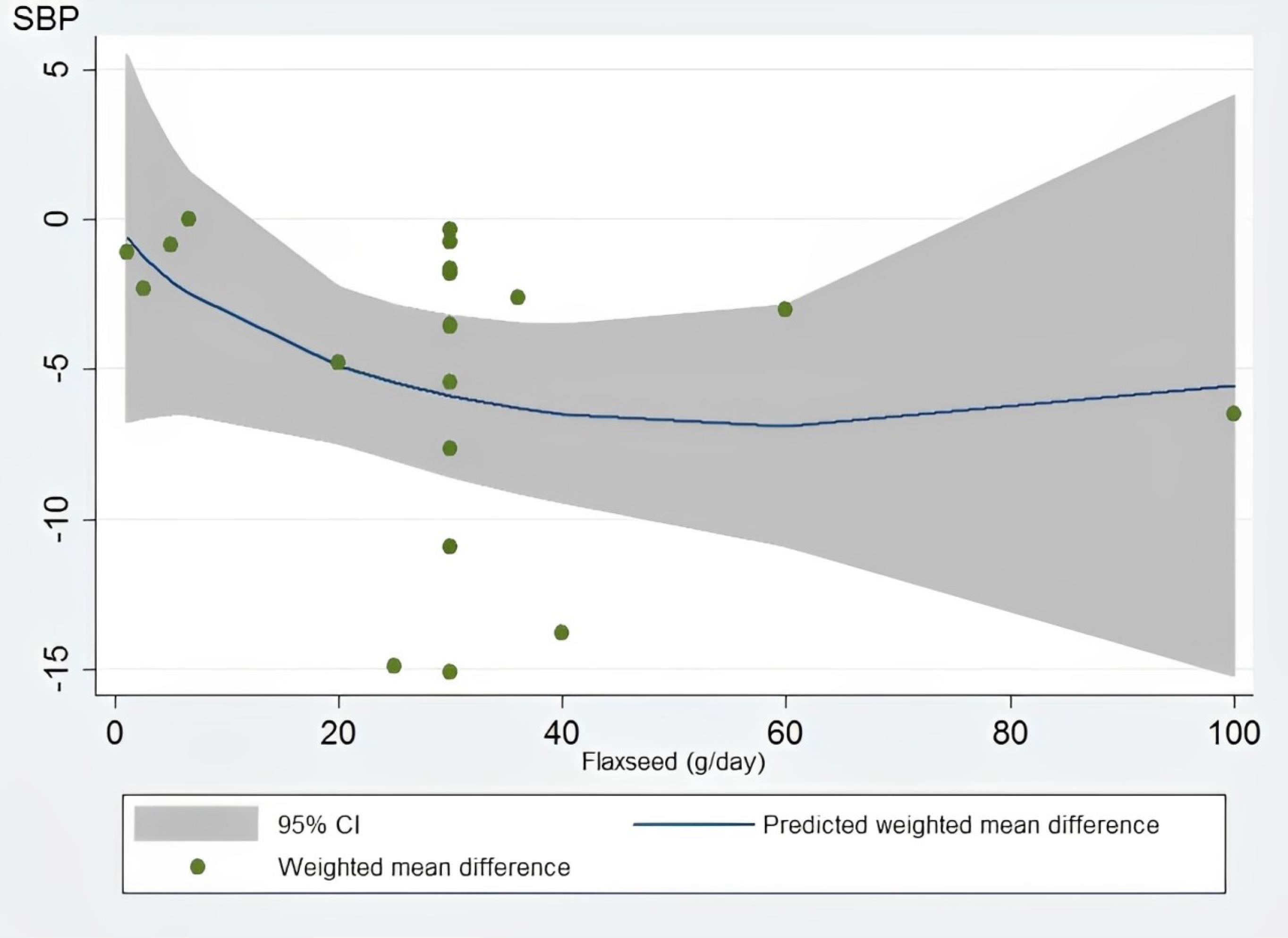
Figure 4.
Non-linear dose-responses between flaxseed and weighted mean difference in systolic blood pressure (mmHg). The 95% confidence interval (CI) is depicted in the shaded regions.
.
Non-linear dose-responses between flaxseed and weighted mean difference in systolic blood pressure (mmHg). The 95% confidence interval (CI) is depicted in the shaded regions.
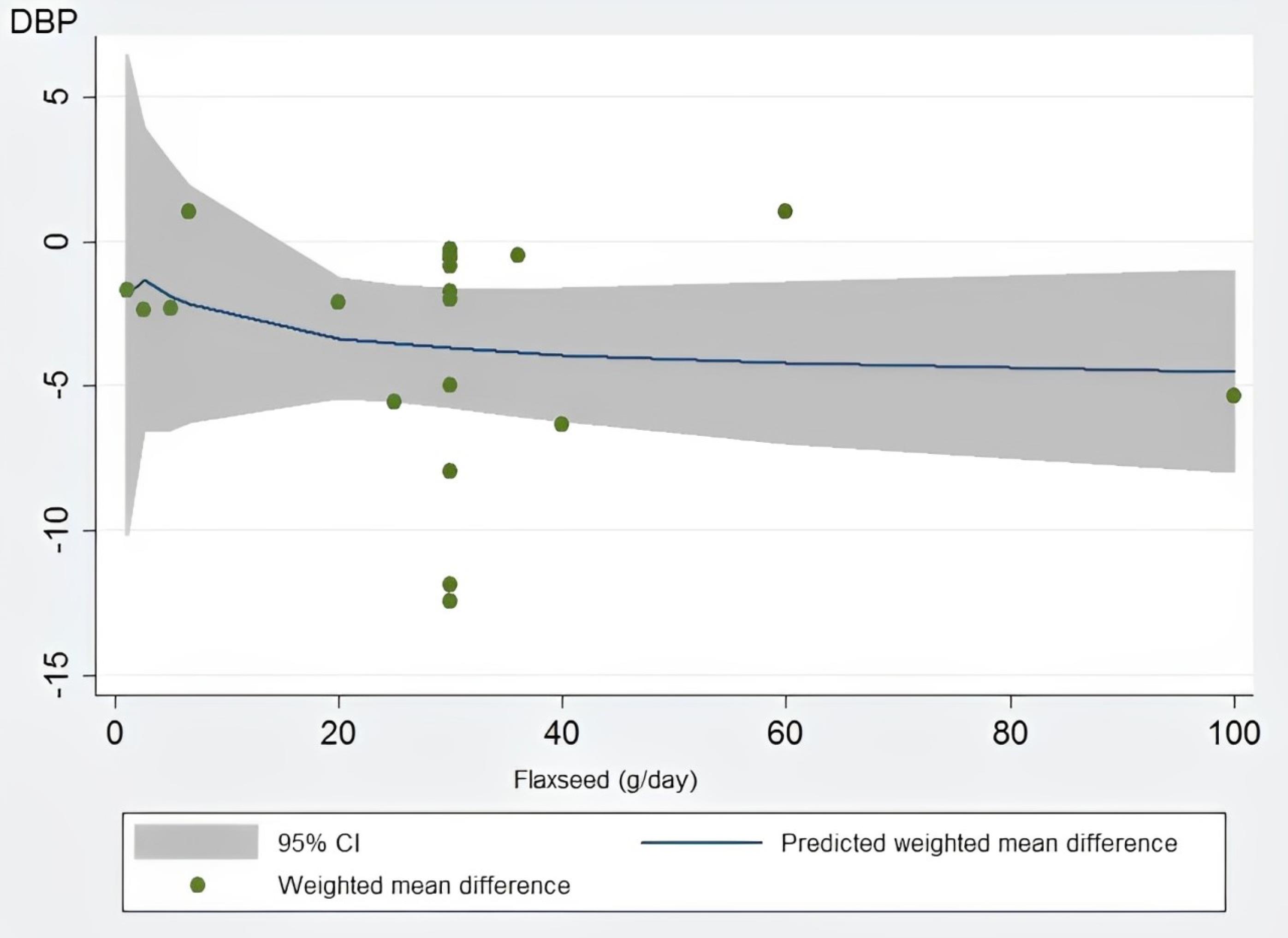
Figure 5.
Non-linear dose-responses between flaxseed and weighted mean difference in diastolic blood pressure (mmHg). The 95% confidence interval (CI) is depicted in the shaded regions
.
Non-linear dose-responses between flaxseed and weighted mean difference in diastolic blood pressure (mmHg). The 95% confidence interval (CI) is depicted in the shaded regions
Sensitivity analysis and publication bias
After systematically removing each study, it was found that the overall effects of flaxseed supplementation on both outcomes were not significantly altered. Egger’s regression asymmetry test for the assessment of the publication bias was performed in the present meta-analysis. The results showed no evidence of publication bias in the studies that examined the effect of flaxseed supplementation on SBP (P = 0.05) and DBP (P = 0.05).
Discussion
This meta-analysis included 18 RCTs that assessed the effect of flaxseed supplementation on BP in patients with CVD risk factors. The combined effects of these trials showed that there were significant differences in SBP and DBP reduction with flaxseed supplementation as compared to the control group. But, it must be mentioned that the heterogeneity across the studies included was very high and by subgrouping only in some subsets the heterogeneity was decreased. For further studies, it should be noted that the interpretation of subgroups should be interpreted with care due to the low power of the subgroup analyses.
The results of this meta-analysis are consistent with three previous meta-analyses47-49 that investigated the BP-lowering effects of flaxseed in adults. However, unlike those studies, the present analysis excluded healthy subjects. On the other hand, a different meta-analysis53 focused specifically on patients with MetS and related disorders and found that flaxseed can lower SBP, but does not affect DBP. The discrepancies between the results of different meta-analyses on the anti-hypertensive properties of flaxseed may stem from differences in the study participants. It stands to reason that flaxseed may not produce the same effects in individuals who are healthy as in those who have health issues. Additionally, individuals with HTN may experience more significant reductions in their BP levels as a result of consuming flaxseed.
The underlying mechanisms responsible for the reduction of BP attributed to flaxseed remain inadequately elucidated. It is hypothesized that multiple factors may play a role in this reduction, encompassing a cardiac depressant action, a diuretic effect, and the presence of calcium channel-blocking attributes.40,54,55 Flaxseed is abundant in ligands, dietary fibers, and phytoestrogens, all of which have demonstrated efficacy in the modulation of BP through a variety of mechanisms.47 The alpha-linolenic acid (ALA) found in flaxseeds has the capacity to induce vasodilation, consequently resulting in a decrease in BP.56 Flaxseed possesses the remarkable ability to lower BP through a multifaceted mechanism that involves the modulation of blood lipid profiles, the augmentation of insulin resistance, as well as the promotion of beneficial gut microflora, all of which can be attributed to the presence of its soluble fiber components.53,57 Furthermore, flaxseed meal protein contains peptide bonds rich in arginine, which can help in generating nitric oxide and other biochemical reactions to improve BP levels.48,58
The results indicate that flaxseed supplementation has a positive effect on BP in patients with CVD risk factors. This improvement in BP may help alleviate the clinical and public health issues associated with HTN and its related complications. Stamler et al59 demonstrated that even a reduction of 2 to 3 mmHg in SBP can result in a 4% decrease in CVD mortality. Additionally, Ogihara et al60 reported that such a reduction in SBP can lead to a 6.4% decrease in mortality from cerebrovascular disease. Therefore, based on the average effect size observed in this study, it can be concluded that the BP-lowering effects of flaxseed are both clinically significant and highly effective. Eventually, flaxseed can be an auxiliary option for people with cardiovascular risk factors, in conjunction with their diet and BP medications.
Flaxseed is predominantly regarded as safe for ingestion, as research conducted on both animal models and human subjects has not indicated the occurrence of significant adverse effects. Nonetheless, excessive consumption of flaxseed may lead to detrimental outcomes such as diarrhea and hypersensitivity reactions. People with coagulation disorders, as well as pregnant or breastfeeding women and children, should consume flaxseed and its derivatives with caution.53,61
Given the identified limitations, it is crucial to evaluate the findings from this comprehensive meta-analysis with caution. Initially, the study groups had a diverse composition, meaning that the research included subjects with various demographic and clinical characteristics, such as differing ages, genders, types of interventions, and initial health statuses. It is of particular significance to acknowledge this in relation to BP levels, given that certain participants in the study exhibited normotensive characteristics while others presented with hypertensive conditions. Secondly, BP was assessed as a secondary outcome in the majority of studies, which may have exerted an influence on the results. Thirdly, the disparate effects of flaxseed on male and female subjects remain undetermined, as the majority of studies included both genders of participants together. Ultimately, the majority of trials failed to report or analyze confounding factors and their corresponding impacts, thereby inhibiting their evaluation in our study. Due to processing delays for submissions pertaining to studies conducted outside the UK, we did not formally register the protocol for the present study in the PROSPERO registry. This lack of registration may potentially introduce a source of bias within the scope of this review. Notwithstanding this limitation, we meticulously formulated and conducted this review and meta-analysis in accordance with Cochrane guidelines.
Conclusion
This comprehensive meta-analysis of RCTs revealed substantial decreases in both SBP and DBP as a result of flaxseed supplementation. Given the significant heterogeneity, it is crucial to interpret the current results with careful consideration. In addition, the mechanisms behind this effect remain to be elucidated. Consequently, it is pertinent to undertake studies with a long duration, particularly among individuals diagnosed with HTN, to ascertain the potential for any interactions, whether advantageous or adverse, with the standard pharmacological treatment protocols for HTN.
Competing Interests
The authors assert the absence of any potential conflicts of interest.
Ethical Approval
The investigation constitutes a comprehensive systematic review and meta-analysis; therefore, ethical approval was not deemed necessary.
Supplementary Files
Table S1. Search terms
(pdf)
Acknowledgements
The authors are thankful to the Deanship of Research and Graduate Studies, King Khalid University, Abha, Saudi Arabia, for financially supporting this work through the Large Research Group Project under Grant no. R.G.P.2/517/45.
References
- Mensah GA, Fuster V, Murray CJL, Roth GA. Global burden of cardiovascular diseases and risks, 1990-2022. J Am Coll Cardiol 2023; 82(25):2350-473. doi: 10.1016/j.jacc.2023.11.007 [Crossref] [ Google Scholar]
- Magnussen C, Ojeda FM, Leong DP, Alegre-Diaz J, Amouyel P, Aviles-Santa L. Global effect of modifiable risk factors on cardiovascular disease and mortality. N Engl J Med 2023; 389(14):1273-85. doi: 10.1056/NEJMoa2206916 [Crossref] [ Google Scholar]
- World Health Organization (WHO). Global Report on Hypertension: The Race Against a Silent Killer. WHO; 2023. Available from: https://www.who.int/publications/i/item/9789240081062.
- Laar AK, Adler AJ, Kotoh AM, Legido-Quigley H, Lange IL, Perel P. Health system challenges to hypertension and related non-communicable diseases prevention and treatment: perspectives from Ghanaian stakeholders. BMC Health Serv Res 2019; 19(1):693. doi: 10.1186/s12913-019-4571-6 [Crossref] [ Google Scholar]
- Valenzuela PL, Carrera-Bastos P, Gálvez BG, Ruiz-Hurtado G, Ordovas JM, Ruilope LM. Lifestyle interventions for the prevention and treatment of hypertension. Nat Rev Cardiol 2021; 18(4):251-75. doi: 10.1038/s41569-020-00437-9 [Crossref] [ Google Scholar]
- Alpsoy Ş. Exercise and hypertension. Adv Exp Med Biol 2020; 1228:153-67. doi: 10.1007/978-981-15-1792-1_10 [Crossref] [ Google Scholar]
- Poulter NR, Borghi C, Parati G, Pathak A, Toli D, Williams B. Medication adherence in hypertension. J Hypertens 2020; 38(4):579-87. doi: 10.1097/hjh.0000000000002294 [Crossref] [ Google Scholar]
- Hunter PG, Chapman FA, Dhaun N. Hypertension: current trends and future perspectives. Br J Clin Pharmacol 2021; 87(10):3721-36. doi: 10.1111/bcp.14825 [Crossref] [ Google Scholar]
- Verma N, Rastogi S, Chia YC, Siddique S, Turana Y, Cheng HM. Non-pharmacological management of hypertension. J Clin Hypertens (Greenwich) 2021; 23(7):1275-83. doi: 10.1111/jch.14236 [Crossref] [ Google Scholar]
- Kota V, Kumar S, Wanjari AK, Acharya S. Lifestyle modification and nutrition in preventing prehypertension and hypertension—narrative review. Int J Nutr Pharmacol Neurol Dis 2023; 13(1):9-15. doi: 10.4103/ijnpnd.ijnpnd_84_22 [Crossref] [ Google Scholar]
- Balaji PA, Smitha RV. Integrated review of management of hypertension by lifestyle changes, yoga, exercise, acupressure, plant/herbal and allopathic medications and newer interventions. Indian J Integr Med 2023; 3(1):1-8. [ Google Scholar]
- Kamyab R, Namdar H, Torbati M, Ghojazadeh M, Araj-Khodaei M, Fazljou SM. Medicinal plants in the treatment of hypertension: a review. Adv Pharm Bull 2021; 11(4):601-17. doi: 10.34172/apb.2021.090 [Crossref] [ Google Scholar]
- Golpour-Hamedani S, Hadi A, Safari Malekabadi D, Najafgholizadeh A, Askari G, Pourmasoumi M. The effect of nigella supplementation on blood pressure: a systematic review and dose-response meta-analysis. Crit Rev Food Sci Nutr 2024; 64(4):943-56. doi: 10.1080/10408398.2022.2110566 [Crossref] [ Google Scholar]
- Hadi A, Askarpour M, Miraghajani M, Symonds ME, Sheikhi A, Ghaedi E. Effects of strawberry supplementation on cardiovascular risk factors: a comprehensive systematic review and meta-analysis of randomized controlled trials. Food Funct 2019; 10(11):6987-98. doi: 10.1039/c9fo01684h [Crossref] [ Google Scholar]
- Ghaffari S, Roshanravan N. The role of nutraceuticals in prevention and treatment of hypertension: an updated review of the literature. Food Res Int 2020; 128:108749. doi: 10.1016/j.foodres.2019.108749 [Crossref] [ Google Scholar]
- Lipert A, Szadkowska I, Matusiak-Wieczorek E, Kochan E. The effect of herbal supplements on blood pressure: systematic review and meta-analysis. Antioxidants (Basel) 2022; 11(8):1419. doi: 10.3390/antiox11081419 [Crossref] [ Google Scholar]
- Pourmasoumi M, Hadi A, Najafgholizadeh A, Kafeshani M, Sahebkar A. Clinical evidence on the effects of saffron (Crocus sativus L) on cardiovascular risk factors: a systematic review meta-analysis. Pharmacol Res 2019; 139:348-59. doi: 10.1016/j.phrs.2018.11.038 [Crossref] [ Google Scholar]
- Shayan M, Kamalian S, Sahebkar A, Tayarani-Najaran Z. Flaxseed for health and disease: review of clinical trials. Comb Chem High Throughput Screen 2020; 23(8):699-722. doi: 10.2174/1386207323666200521121708 [Crossref] [ Google Scholar]
- Jalili C, Pezeshki M, Askarpour M, Marx W, Hassani B, Hadi A. The effect of flaxseed supplementation on circulating adiponectin and leptin concentration in adults: a systematic review and meta-analysis of randomized controlled trials. Phytother Res 2020; 34(7):1578-86. doi: 10.1002/ptr.6634 [Crossref] [ Google Scholar]
- Yasmeen M, Nisar S, Tavallali V, Khalid T. A review of phytochemicals and uses of flaxseed. Int J Chem Biochem Sci 2018; 13:70-5. [ Google Scholar]
- Askarpour M, Karimi M, Hadi A, Ghaedi E, Symonds ME, Miraghajani M. Effect of flaxseed supplementation on markers of inflammation and endothelial function: a systematic review and meta-analysis. Cytokine 2020; 126:154922. doi: 10.1016/j.cyto.2019.154922 [Crossref] [ Google Scholar]
- Hadi A, Askarpour M, Salamat S, Ghaedi E, Symonds ME, Miraghajani M. Effect of flaxseed supplementation on lipid profile: an updated systematic review and dose-response meta-analysis of sixty-two randomized controlled trials. Pharmacol Res 2020; 152:104622. doi: 10.1016/j.phrs.2019.104622 [Crossref] [ Google Scholar]
- Hadi A, Askarpour M, Ziaei R, Venkatakrishnan K, Ghaedi E, Ghavami A. Impact of flaxseed supplementation on plasma lipoprotein(a) concentrations: a systematic review and meta-analysis of randomized controlled trials. Phytother Res 2020; 34(7):1599-608. doi: 10.1002/ptr.6640 [Crossref] [ Google Scholar]
- Mohammadi-Sartang M, Mazloom Z, Raeisi-Dehkordi H, Barati-Boldaji R, Bellissimo N, Totosy de Zepetnek JO. The effect of flaxseed supplementation on body weight and body composition: a systematic review and meta-analysis of 45 randomized placebo-controlled trials. Obes Rev 2017; 18(9):1096-107. doi: 10.1111/obr.12550 [Crossref] [ Google Scholar]
- Xi H, Zhou W, Sohaib M, Niu Y, Zhu R, Guo Y. Flaxseed supplementation significantly reduces hemoglobin A1c in patients with type 2 diabetes mellitus: a systematic review and meta-analysis. Nutr Res 2023; 110:23-32. doi: 10.1016/j.nutres.2022.12.008 [Crossref] [ Google Scholar]
- Akter Y, Junaid M, Afrose SS, Nahrin A, Alam MS, Sharmin T. A comprehensive review on Linumusitatissimum medicinal plant: its phytochemistry, pharmacology, and ethnomedicinal uses. Mini Rev Med Chem 2021; 21(18):2801-34. doi: 10.2174/1389557521666210203153436 [Crossref] [ Google Scholar]
- Bhavana KB, Babu AN, Lakshmi J, Deepthi B, Kavya G. A review on pharmacological properties and laboratory outcomes of flaxseed diet (Linumusitatissimum). Int J Pharm Sci Rev Res 2021; 70(1):100-5. doi: 10.47583/ijpsrr.2021.v70i01.013 [Crossref] [ Google Scholar]
- Patel KP, Patel S, Dash DK, Balaraman R, Maheshwari RA. A review on flax seed: a legume for longevity. J Pharm Res Int 2021; 33(39A):107-22. doi: 10.9734/JPRI/2021/v33i39A32148 [Crossref] [ Google Scholar]
- Akrami A, Nikaein F, Babajafari S, Faghih S, Yarmohammadi H. Comparison of the effects of flaxseed oil and sunflower seed oil consumption on serum glucose, lipid profile, blood pressure, and lipid peroxidation in patients with metabolic syndrome. J Clin Lipidol 2018; 12(1):70-7. doi: 10.1016/j.jacl.2017.11.004 [Crossref] [ Google Scholar]
- Bhardwaj K, Verma N, Trivedi R, Bhardwaj S. Effect of essential fatty acid blend on circadian variations of ambulatory blood pressure in patients with essential hypertension and coronary artery disease risk markers. J Hum Hypertens 2022; 36(3):289-98. doi: 10.1038/s41371-021-00520-9 [Crossref] [ Google Scholar]
- Cassani RS, Fassini PG, Silvah JH, Lima CM, Marchini JS. Impact of weight loss diet associated with flaxseed on inflammatory markers in men with cardiovascular risk factors: a clinical study. Nutr J 2015; 14:5. doi: 10.1186/1475-2891-14-5 [Crossref] [ Google Scholar]
- Dewell A, Marvasti FF, Harris WS, Tsao P, Gardner CD. Low- and high-dose plant and marine (n-3) fatty acids do not affect plasma inflammatory markers in adults with metabolic syndrome. J Nutr 2011; 141(12):2166-71. doi: 10.3945/jn.111.142240 [Crossref] [ Google Scholar]
- Haghighatsiar N, Askari G, Saraf-Bank S, Feizi A, Keshmiri H. Effect of flaxseed powder on cardiovascular risk factor in dyslipidemic and hypertensive patients. Int J Prev Med 2019; 10:218. doi: 10.4103/ijpvm.IJPVM_563_17 [Crossref] [ Google Scholar]
- Hasaniani N, Rahimlou M, Ramezani Ahmadi A, Mehdizadeh Khalifani A, Alizadeh M. The effect of flaxseed enriched yogurt on the glycemic status and cardiovascular risk factors in patients with type 2 diabetes mellitus: randomized, open-labeled, controlled study. Clin Nutr Res 2019; 8(4):284-95. doi: 10.7762/cnr.2019.8.4.284 [Crossref] [ Google Scholar]
- Javidi A, Mozaffari-Khosravi H, Nadjarzadeh A, Dehghani A, Eftekhari MH. The effect of flaxseed powder on insulin resistance indices and blood pressure in prediabetic individuals: a randomized controlled clinical trial. J Res Med Sci 2016; 21:70. doi: 10.4103/1735-1995.189660 [Crossref] [ Google Scholar]
- Katare C, Saxena S. Amelioration of selected cardiac risk factors through supplementation of diet with flaxseed and soya bean. Int J Nutr Pharmacol Neurol Dis 2013; 3(4):352-7. doi: 10.4103/2231-0738.119844 [Crossref] [ Google Scholar]
- Kuang X, Kong Y, Hu X, Li K, Guo X, Liu C. Defatted flaxseed flour improves weight loss and lipid profile in overweight and obese adults: a randomized controlled trial. Food Funct 2020; 11(9):8237-47. doi: 10.1039/d0fo00838a [Crossref] [ Google Scholar]
- Pieters DJ, Zock PL, Fuchs D, Mensink RP. Effect of α-linolenic acid on 24-h ambulatory blood pressure in untreated high-normal and stage I hypertensive subjects. Br J Nutr 2019; 121(2):155-63. doi: 10.1017/s0007114518003094 [Crossref] [ Google Scholar]
- Rezaei S, Sasani MR, Akhlaghi M, Kohanmoo A. Flaxseed oil in the context of a weight loss programme ameliorates fatty liver grade in patients with non-alcoholic fatty liver disease: a randomised double-blind controlled trial. Br J Nutr 2020; 123(9):994-1002. doi: 10.1017/s0007114520000318 [Crossref] [ Google Scholar]
- Rodriguez-Leyva D, Weighell W, Edel AL, LaVallee R, Dibrov E, Pinneker R. Potent antihypertensive action of dietary flaxseed in hypertensive patients. Hypertension 2013; 62(6):1081-9. doi: 10.1161/hypertensionaha.113.02094 [Crossref] [ Google Scholar]
- Saleh-Ghadimi S, Kheirouri S, Golmohammadi A, Moludi J, Jafari-Vayghan H, Alizadeh M. Effect of flaxseed oil supplementation on anthropometric and metabolic indices in patients with coronary artery disease: a double-blinded randomized controlled trial. J Cardiovasc Thorac Res 2019; 11(2):152-60. doi: 10.15171/jcvtr.2019.26 [Crossref] [ Google Scholar]
- Toulabi T, Yarahmadi M, Goudarzi F, Ebrahimzadeh F, Momenizadeh A, Yarahmadi S. Effects of flaxseed on blood pressure, body mass index, and total cholesterol in hypertensive patients: a randomized clinical trial. Explore (NY) 2022; 18(4):438-45. doi: 10.1016/j.explore.2021.05.003 [Crossref] [ Google Scholar]
- Wu H, Pan A, Yu Z, Qi Q, Lu L, Zhang G. Lifestyle counseling and supplementation with flaxseed or walnuts influence the management of metabolic syndrome. J Nutr 2010; 140(11):1937-42. doi: 10.3945/jn.110.126300 [Crossref] [ Google Scholar]
- Yang B, Shi L, Wang AM, Shi MQ, Li ZH, Zhao F. Lowering effects of n-3 fatty acid supplements on blood pressure by reducing plasma angiotensin ii in inner Mongolia hypertensive patients: a double-blind randomized controlled trial. J Agric Food Chem 2019; 67(1):184-92. doi: 10.1021/acs.jafc.8b05463 [Crossref] [ Google Scholar]
- Yari Z, Cheraghpour M, Hekmatdoost A. Flaxseed and/or hesperidin supplementation in metabolic syndrome: an open-labeled randomized controlled trial. Eur J Nutr 2021; 60(1):287-98. doi: 10.1007/s00394-020-02246-9 [Crossref] [ Google Scholar]
- Yari Z, Rahimlou M, Poustchi H, Hekmatdoost A. Flaxseed supplementation in metabolic syndrome management: a pilot randomized, open-labeled, controlled study. Phytother Res 2016; 30(8):1339-44. doi: 10.1002/ptr.5635 [Crossref] [ Google Scholar]
- Khalesi S, Irwin C, Schubert M. Flaxseed consumption may reduce blood pressure: a systematic review and meta-analysis of controlled trials. J Nutr 2015; 145(4):758-65. doi: 10.3945/jn.114.205302 [Crossref] [ Google Scholar]
- Ursoniu S, Sahebkar A, Andrica F, Serban C, Banach M. Effects of flaxseed supplements on blood pressure: a systematic review and meta-analysis of controlled clinical trial. Clin Nutr 2016; 35(3):615-25. doi: 10.1016/j.clnu.2015.05.012 [Crossref] [ Google Scholar]
- Li L, Li H, Gao Y, Vafaei S, Zhang X, Yang M. Effect of flaxseed supplementation on blood pressure: a systematic review, and dose-response meta-analysis of randomized clinical trials. Food Funct 2023; 14(2):675-90. doi: 10.1039/d2fo02566c [Crossref] [ Google Scholar]
- Moher D, Liberati A, Tetzlaff J, Altman DG. Preferred reporting items for systematic reviews and meta-analyses: the PRISMA statement. Ann Intern Med 2009; 151(4):264-9. doi: 10.7326/0003-4819-151-4-200908180-00135 [Crossref] [ Google Scholar]
- Higgins JP. The Cochrane Collaboration’s Tool for Assessing Risk of Bias in Randomised Trials. The Cochrane Collaboration; 2011.
- Guyatt GH, Oxman AD, Vist GE, Kunz R, Falck-Ytter Y, Alonso-Coello P. GRADE: an emerging consensus on rating quality of evidence and strength of recommendations. BMJ 2008; 336(7650):924-6. doi: 10.1136/bmj.39489.470347.AD [Crossref] [ Google Scholar]
- Mahmudiono T, Jasim SA, Karim YS, Bokov DO, Abdelbasset WK, Akhmedov KS. The effect of flaxseed oil consumtion on blood pressure among patients with metabolic syndrome and related disorders: a systematic review and meta-analysis of randomized clinical trials. Phytother Res 2022; 36(10):3766-73. doi: 10.1002/ptr.7566 [Crossref] [ Google Scholar]
- Caligiuri SP, Rodriguez-Leyva D, Aukema HM, Ravandi A, Weighell W, Guzman R. Dietary flaxseed reduces central aortic blood pressure without cardiac involvement but through changes in plasma oxylipins. Hypertension 2016; 68(4):1031-8. doi: 10.1161/hypertensionaha.116.07834 [Crossref] [ Google Scholar]
- Palla AH, Rehman NU, Siddiqi HS, Gilani AU, Siddiqui BS, Perwaiz MI. Cardiac depressant and vasodialatory effect of flaxseed-basis for the medicinal use in hypertension. Sains Malays 2021; 50(9):2687-700. doi: 10.17576/jsm-2021-5009-16 [Crossref] [ Google Scholar]
- Bertoni C, Abodi M, D’Oria V, Milani GP, Agostoni C, Mazzocchi A. Alpha-linolenic acid and cardiovascular events: a narrative review. Int J Mol Sci 2023; 24(18):14319. doi: 10.3390/ijms241814319 [Crossref] [ Google Scholar]
- Prasad K. Importance of flaxseed and its components in the management of hypertension. Int J Angiol 2019; 28(3):153-60. doi: 10.1055/s-0039-1678691 [Crossref] [ Google Scholar]
- Udenigwe CC, Adebiyi AP, Doyen A, Li H, Bazinet L, Aluko RE. Low molecular weight flaxseed protein-derived arginine-containing peptides reduced blood pressure of spontaneously hypertensive rats faster than amino acid form of arginine and native flaxseed protein. Food Chem 2012; 132(1):468-75. doi: 10.1016/j.foodchem.2011.11.024 [Crossref] [ Google Scholar]
- Stamler J, Rose G, Stamler R, Elliott P, Dyer A, Marmot M. INTERSALT study findings Public health and medical care implications. Hypertension 1989; 14(5):570-7. doi: 10.1161/01.hyp.14.5.570 [Crossref] [ Google Scholar]
- Ogihara T, Kikuchi K, Matsuoka H, Fujita T, Higaki J, Horiuchi M. The Japanese Society of Hypertension guidelines for the management of hypertension (JSH 2009). Hypertens Res 2009; 32(1):3-107. [ Google Scholar]
- Amin T, Thakur M. Linumusitatissimum L(flaxseed)–a multifarious functional food. Online International Interdisciplinary Research Journal 2014; 4(1):220-38. [ Google Scholar]